There is a healthy debate over whether a lab that created an extremely infectious version of influenza ought to publish the genetic sequence. The debate speaks to a larger problem: sometimes, medical advances do the world a disservice. The medical field could use some soul-searching, just as physicists did in the wake of the Manhattan Project.
A few years ago, I read a neat research finding: in a pregnant woman, some of the fetus's DNA crosses the placenta and circulates in the mother's bloodstream. Drawing on this finding, some researchers developed a clever blood test that is allowing pregnant women to non-invasively screen their fetuses for Down Syndrome (whereas in the past, amniocentesis or chorionic villus sampling were the definitive screens). Good on them.
Yet other researchers have done gone a step further, offering both maternal blood tests and a maternal urine test that reveals a fetus's gender. One of these researchers, Prof. Diana Bianchi of Tufts University, justifies her development of a blood test because it will help mothers receive early warning about whether their children are at risk for genetic, sex-linked conditions such as hemophilia and congential adrenal hyperplasia.
This benefit strikes me as far too small relative to the tests' tremendous downside: it will greatly worsen the calamitous global phenomenon of the Missing Women.
The expected sex ratio at birth is 105 boys born for every 100 girls, or 1.05. Yet in some countries, the sex ratio at birth is quite skewed: for example, China's is 1.13 and Vietnam's is 1.12. What results is a demographic disaster, with over 100 million women missing worldwide (and a number of unhappy single men left in their wake). This glut of unmarried men may even contribute to global unrest, as unmarried men are more likely than married men to engage in armed conflict or become terrorists.
A renowned economist, Amartya Sen, established that cultural bias against women underlies the deficit. In countries where it is economically advantageous to have a boy, some families murder or neglect their infant girls or abort their female fetuses. Currently, ultrasonography is the only non-invasive way to determine the gender of a fetus. Some of the affected countries have forbidden ultrasound clinics from revealing a fetus's gender, and some intermittently crack down on those profitable yet illicit ultrasound clinics that flout the rules.
But a maternal blood test or urine test will prove impossible to regulate. Making it easier for mothers to determine gender will almost certainly lead to more female fetuses being aborted worldwide, with all of its concomitant problems. I would at the very least like to see a fraction of the proceeds for this blood test go to empowering women in affected countries (by boosting primary education and decreasing maternal and infant mortality), which would begin to help the problem. I doubt we will see it.
Some medical disasters are not easily foreseeable. For example, most leading orthopedists did not expect metal-on-metal hip replacements to become a massive fiasco. Yet developing a maternal blood test for fetal gender has so little justification and its ramifications are so potentially terrible that I believe its developers acted unethically. It's a shame that some scientific advances leave the world worse off than before, because I believe that scientific inquiry possesses a unique ability to make the world rather wonderful.
29 December 2011
22 December 2011
Mercury news
Echoing Paul Krugman, I want to point out how huge a deal it is that President Obama and the EPA have issued new national standards limiting heavy-metal emissions from power plants. From the EPA's press release yesterday:
As hard as my classmates and I will try to take care of our patients as physicians, what we can accomplish as individuals cannot come close to the impact of prudent regulations such as this. Bear in mind too that some of the energy sector lobbied hard to prevent these standards from being issued. Good on the Obama administration for protecting the environment and bettering human lives.
The U.S. Environmental Protection Agency (EPA) has issued the Mercury and Air Toxics Standards, the first national standards to protect American families from power plant emissions of mercury and toxic air pollution like arsenic, acid gas, nickel, selenium, and cyanide. The standards will slash emissions of these dangerous pollutants by relying on widely available, proven pollution controls that are already in use at more than half of the nation’s coal-fired power plants.
11,000 premature deaths per year is a big number. By comparison, the CDC attributes 42,000 deaths annually to "motor-vehicle traffic" accidents. The September 11 terrorist attacks caused just under 3,000 premature deaths, once. And mercury is scary stuff. It tends to accumulate in large fish and in mammals that sit atop the food chain. Pregnant women are discouraged from eating certain types of fish (including albacore tuna) because ingesting the amount of mercury they contain can cause birth defects.EPA estimates that the new safeguards will prevent as many as 11,000 premature deaths and 4,700 heart attacks a year. The standards will also help America’s children grow up healthier – preventing 130,000 cases of childhood asthma symptoms and about 6,300 fewer cases of acute bronchitis among children each year. [emphasis mine]
As hard as my classmates and I will try to take care of our patients as physicians, what we can accomplish as individuals cannot come close to the impact of prudent regulations such as this. Bear in mind too that some of the energy sector lobbied hard to prevent these standards from being issued. Good on the Obama administration for protecting the environment and bettering human lives.
18 December 2011
How we learn
I worry somewhat that learning for learning's sake can be a liability in medical school. Perhaps out of necessity, my class devotes the bulk of its energy to excelling on exams. Sometimes this drive to perform runs counter to learning: one of the most effective study tools is to obtain old copies of quizzes and exams. One can do quite well by memorizing the answers to questions that historically appear on exams, even without understanding quite what they mean. Another winning strategy is to come up with mnemonics particular to the examination ("The four arteries we were supposed to remember begin with the letters MIDS").
It makes sense why some classmates would opt to limit their studying to what will be assessed on exams and boards. Many have girlfriends, boyfriends, spouses, and children that (deservedly) compete for their energy and time. Getting top marks in courses yields academic distinction and hefty scholarships. Even our class's lingo revolves around the test: topics likely to appear on an exam are termed "high-yield." Wasting classmates' time with "low-yield" topics is a cardinal sin. Few students read the assigned textbooks, because the exam material derives from the bolded bullet points in our lectures' PowerPoint slides. We were told ahead of time exactly which physical examination methods we needed to know on the final exam; others were summarily ignored.
Even the boards that we take second year (the standardized examination that all allopathic medical students take, and that plays heavily into residency placements) promote shortcuts. If a question begins: "A 19-year old female sex worker comes into your clinic," I instantly know that the answer they will want me to put is a type of STI. Real life is not so simple. Clinical decisions do not involve choosing the best answer of the five choices proferred.
The fundamental question is: should we consider medical school an educational experience in its own right? Or should we treat it as a stepping-stone to our desired residency and career? I fear that learning to the test prevents us from becoming that breed of excellent physician that inspired me to enter the profession.
It makes sense why some classmates would opt to limit their studying to what will be assessed on exams and boards. Many have girlfriends, boyfriends, spouses, and children that (deservedly) compete for their energy and time. Getting top marks in courses yields academic distinction and hefty scholarships. Even our class's lingo revolves around the test: topics likely to appear on an exam are termed "high-yield." Wasting classmates' time with "low-yield" topics is a cardinal sin. Few students read the assigned textbooks, because the exam material derives from the bolded bullet points in our lectures' PowerPoint slides. We were told ahead of time exactly which physical examination methods we needed to know on the final exam; others were summarily ignored.
Even the boards that we take second year (the standardized examination that all allopathic medical students take, and that plays heavily into residency placements) promote shortcuts. If a question begins: "A 19-year old female sex worker comes into your clinic," I instantly know that the answer they will want me to put is a type of STI. Real life is not so simple. Clinical decisions do not involve choosing the best answer of the five choices proferred.
The fundamental question is: should we consider medical school an educational experience in its own right? Or should we treat it as a stepping-stone to our desired residency and career? I fear that learning to the test prevents us from becoming that breed of excellent physician that inspired me to enter the profession.
'Smallpox: The Death of a Disease', by D.A. Henderson
D.A. Henderson led the WHO office that coordinated the global smallpox eradication effort. His 2009 book focuses on the bureaucratic and diplomatic challenges that he and his shoestring staff had to overcome to combat the disease. He gives of an overview of how eradication unfolded in each of the endemic countries, including Bangladesh, which was torn by civil war, and Ethiopia, which had poor infrastructure and a substantial population of nomads. Despite seemingly insurmountable challenges, even the poorest countries accomplished this extraordinary public health feat. Young health care professionals bounding with creativity and ingenuity ultimately prevailed. Henderson also discusses the evolving debate over whether to destroy the remaining stockpiles of smallpox, as well as the threat of a bioterrorism attack involving smallpox. Henderson's work propelled him to a distinguished career as dean of the Johns Hopkins School of Public Health and as a senior White House administrator.
"Smallpox: The Death of a Disease" is a more academic and bird's-eye view of smallpox eradication than is William Foege's "House on Fire: The Fight to Eradicate Smallpox" (which I reviewed earlier). I would recommend first reading "House on Fire." If you find that book particularly stimulating, you will likely enjoy Henderson's book, as I did.
"Smallpox: The Death of a Disease" is a more academic and bird's-eye view of smallpox eradication than is William Foege's "House on Fire: The Fight to Eradicate Smallpox" (which I reviewed earlier). I would recommend first reading "House on Fire." If you find that book particularly stimulating, you will likely enjoy Henderson's book, as I did.
17 December 2011
'House on Fire: The Fight to Eradicate Smallpox', by William Foege
William Foege, a physician who went on to become Director of the Centers for Disease Control, recently wrote memoirs of his experiences leading the smallpox eradication efforts in Nigeria and India. Foege pioneered the successful "surveillance and containment" eradication strategy, which let health teams avoid vaccinating the entire population. Instead, dedicated search teams located infections, and containment teams vaccinated those cities that were sites of outbreaks. Using this method, smallpox was eradicated worldwide in the 1970's. Interestingly, eradication saved the U.S. a substantial amount of money--what it spent on smallpox eradication was only a fraction of what it spent each year on domestic vaccination and on verifying that travelers to the U.S. were immune. It's important to note the debt owed to many countries, including the U.S.S.R., which first championed global eradication and donated a tremendous amount of vaccine.
Given how deadly, disfiguring, and persistent smallpox was worldwide, its eradication is perhaps the proudest accomplishment of global public health. Foege's account illustrates how this monumental effort succeeded only because of scrupulous planning, careful research, a shared vision among health workers, and several strokes of good luck. He writes of his experiences in Nigeria, where civil war broke out, and in India, the leaders of which were largely skeptical of eradication.
I found the book fascinating, insightful, and brief. I strongly recommend it to those interested in public health, health systems management, and infectious disease.
Given how deadly, disfiguring, and persistent smallpox was worldwide, its eradication is perhaps the proudest accomplishment of global public health. Foege's account illustrates how this monumental effort succeeded only because of scrupulous planning, careful research, a shared vision among health workers, and several strokes of good luck. He writes of his experiences in Nigeria, where civil war broke out, and in India, the leaders of which were largely skeptical of eradication.
I found the book fascinating, insightful, and brief. I strongly recommend it to those interested in public health, health systems management, and infectious disease.
16 December 2011
Why policy matters
You may have read that the U.S. is mired in a shortage of many common generic drugs. Many important chemotherapy drugs are in such short supply that patients cannot complete their cancer treatments, or are being switched to less appropriate or more expensive treatments. Some drug trials have been suspended because the control group is not able to receive the standard of care.
The severity of the shortage is startling. It also deserves some introspection. Our government spends a tremendous amount on researching new drugs (the NIH estimates that it alone spends $31.2 billion annually on medical research). Why aren't we devoting more of our efforts to manufacturing and delivering those inexpensive drugs that we already know to be effective?
Better policies could have prevented such a shortage. Part of the problem seems to be that Medicare is required to pay such low prices for generic drugs that there is little profit margin for manufacturers, and thus, little incentive to invest in maintaining factories and in keeping up production. If Congress were to nudge the reimbursement rate for generic drugs slightly upwards, Medicare would probably save money overall by avoiding expensive shortages. There also may be something more insidious going on, in which manufacturers and middlemen find it profitable to limit supply and thus drive up prices (much like Enron did with California's electrical supply in 2000 and 2001). The government could also develop stronger penalties if drug manufacturers fail to fulfill their contracts to supply drugs to federal health entities (such as the VA and the Indian Health Service).
Medicine does not occur in a vacuum, and this shortage should be another wake-up call that it behooves doctors and patients to understand more broadly what impacts our nation's health and medical care. After all, any of us may become the patients so desperately needing these drugs.
The severity of the shortage is startling. It also deserves some introspection. Our government spends a tremendous amount on researching new drugs (the NIH estimates that it alone spends $31.2 billion annually on medical research). Why aren't we devoting more of our efforts to manufacturing and delivering those inexpensive drugs that we already know to be effective?
Better policies could have prevented such a shortage. Part of the problem seems to be that Medicare is required to pay such low prices for generic drugs that there is little profit margin for manufacturers, and thus, little incentive to invest in maintaining factories and in keeping up production. If Congress were to nudge the reimbursement rate for generic drugs slightly upwards, Medicare would probably save money overall by avoiding expensive shortages. There also may be something more insidious going on, in which manufacturers and middlemen find it profitable to limit supply and thus drive up prices (much like Enron did with California's electrical supply in 2000 and 2001). The government could also develop stronger penalties if drug manufacturers fail to fulfill their contracts to supply drugs to federal health entities (such as the VA and the Indian Health Service).
Medicine does not occur in a vacuum, and this shortage should be another wake-up call that it behooves doctors and patients to understand more broadly what impacts our nation's health and medical care. After all, any of us may become the patients so desperately needing these drugs.
14 December 2011
A milestone
I have successfully completed my first semester of medical school. This means that I am approximately a tenth of the way towards receiving a license to practice medicine (four years of medical school and a subsequent year of internship). I have learned much, yet I feel like I know only the tiniest fraction of what a good physician ought to.
Next semester we will begin studying the ways the body becomes diseased and the treatments for those illnesses. I wonder, after completing my next final exams in six months, how much closer I'll feel to being a doctor.
Next semester we will begin studying the ways the body becomes diseased and the treatments for those illnesses. I wonder, after completing my next final exams in six months, how much closer I'll feel to being a doctor.
02 December 2011
Resemblance
Sir Ernest Shackleton, the famed Antarctic explorer, climbed in 1915 across then-unexplored South Georgia Island with two members of his shipwrecked expedition. Famished, freezing, thirsty, exhausted, and underequipped, their desperate journey was their last hope of reaching civilization (in the form of a whaling station on the other side of the ice-encrusted, mountainous island). There, they hoped to inform the outside world of their comrades who were stranded on Antarctica and needing a rescue.
In his excellent memoir, South, Shackleton recalled his perception of someone accompanying the men during their harrowing tramp:
I know that during that long and racking march of thirty-six hours over the unnamed mountains and glaciers of South Georgia it seemed to me often that we were four, not three. I said nothing to my companions on the point, but afterwards Worsley said to me, "Boss, I had a curious feeling on the march that there was another person with us." Crean confessed to the same idea. One feels "the dearth of human words, the roughness of mortal speech" in trying to describe things intangible.
Tonight, I was drawing a schematic of a left-to-right ventricular shunt (a type of heart defect) while working out a tough physiology problem. Staring back at me was a smiling Picasso-esque human face, accompanying me as I studied into the wee hours of the night:
I always dreamed of emulating a bold adventurer like Shackleton. Unfortunately, passing my medical school courses lacks the heroics of Shackleton's escape from the Antarctic ice and the eventual rescue of his entire expedition. At least I can dream up some parallels and pretend.
01 December 2011
Exams
The blog will wind down for the next couple of weeks because of our upcoming comprehensive final exams. The amount of material we're responsible for feels staggering. I have never studied this hard in my life. But in going over all that we've learned, I've been delighted to see just how far we have come. I know tremendously more about the human body than I did four months ago. I'm eager to discover what the next few years will hold.
26 November 2011
Charon
The anesthesiology resident who writes at the Asclepion blog has likened his work to that of Charon, the ancient Greek ferryman of the underworld:
An experience in clinic had made me compare my work to Charon's, but in an entirely different way. Given the wonderful ambiguity of some Greek myths, it's only fitting that we'd establish different connections to this same character.
My patient was an impoverished illegal immigrant with a shockingly low potassium level, so low as to be fatal for most people. His blood pressure was also quite elevated. The attending and I whittled down his differential diagnosis until it pointed strongly to primary hyperaldosteronism, an oversecretion of a particular hormone that is often caused by a tumor. We scheduled him for a more extensive work-up.
And yet, beyond treating symptoms, there would probably be little our free clinic could do. We lacked the capacity to perform CT's, MRI's, X-rays, or ultrasounds, any of which we would need to find a tumor. If the presence of a tumor were confirmed, our patient would not be able to afford the life-saving surgery. As an illegal immigrant, he lacked insurance and was ineligible for county services. He could only be admitted to our university hospital if he became so ill that it would be illegal for the ER to discharge him. Entirely because he could not access care, his prognosis looked grim.
Here, I felt like Charon, who ferries people to the underworld. Our laws and medical system prevented us from healing this human being. All I could do was briefly and helplessly accompany him as he traveled to the other side.
Last year, Congress shot down a proposal that would have allowed tax-paying illegal immigrants to purchase health insurance. It's fortunate for our legislators that they don't have to witness the consequences firsthand.
On a happier note, children under 18 are insured by the state and federal government, regardless of immigration status. I haven't seen any in clinic, and that's the way it should be.
I have wondered if anesthesiologists are similar (but distinctly different) mariners [to Charon]. We dare to cross that threshold with the faith that our trips are not one-way. We take those, coin in eye, who have some need of transient depth, who trust us as navigators and cartographers. Are patients the modern day Heracles and Orpheus? Do we carry them across some mythical river and return them safely from their katabasis?
My patient was an impoverished illegal immigrant with a shockingly low potassium level, so low as to be fatal for most people. His blood pressure was also quite elevated. The attending and I whittled down his differential diagnosis until it pointed strongly to primary hyperaldosteronism, an oversecretion of a particular hormone that is often caused by a tumor. We scheduled him for a more extensive work-up.
And yet, beyond treating symptoms, there would probably be little our free clinic could do. We lacked the capacity to perform CT's, MRI's, X-rays, or ultrasounds, any of which we would need to find a tumor. If the presence of a tumor were confirmed, our patient would not be able to afford the life-saving surgery. As an illegal immigrant, he lacked insurance and was ineligible for county services. He could only be admitted to our university hospital if he became so ill that it would be illegal for the ER to discharge him. Entirely because he could not access care, his prognosis looked grim.
Here, I felt like Charon, who ferries people to the underworld. Our laws and medical system prevented us from healing this human being. All I could do was briefly and helplessly accompany him as he traveled to the other side.
Last year, Congress shot down a proposal that would have allowed tax-paying illegal immigrants to purchase health insurance. It's fortunate for our legislators that they don't have to witness the consequences firsthand.
On a happier note, children under 18 are insured by the state and federal government, regardless of immigration status. I haven't seen any in clinic, and that's the way it should be.
20 November 2011
Secret hospitals
My favorite television program, FRONTLINE, recently ran an extraordinary piece on the ongoing Syrian uprising. The reporter went undercover with the underground resistance and experienced firsthand the brutal repression of the Assad regime and the public's noble attempts to gain democracy.
Heartrending for me was the segment on Syria's underground hospitals. Wounded protestors face arrest, torture, and death at the hands of state police if they seek treatment at a public hospital. Doctors who treat protestors risk a similar fate. Sympathetic doctors have improvised, treating seriously-wounded protestors in secret homes, using spartan donated equipment and in constant fear of discovery. This is not what medical care should have to look like. It is a forceful argument for why everyone in our country, including our prisoners, ought to have health care as a basic right. It also argues for non-judgmental regard in medical practice, a complex ethical concept that I haven't entirely come to grips with.
The particular segment on hospitals is below.
I encourage you to watch the entire "Syria Undercover" piece at FRONTLINE's website.
Heartrending for me was the segment on Syria's underground hospitals. Wounded protestors face arrest, torture, and death at the hands of state police if they seek treatment at a public hospital. Doctors who treat protestors risk a similar fate. Sympathetic doctors have improvised, treating seriously-wounded protestors in secret homes, using spartan donated equipment and in constant fear of discovery. This is not what medical care should have to look like. It is a forceful argument for why everyone in our country, including our prisoners, ought to have health care as a basic right. It also argues for non-judgmental regard in medical practice, a complex ethical concept that I haven't entirely come to grips with.
The particular segment on hospitals is below.
Watch Syria Undercover on PBS. See more from FRONTLINE.
I encourage you to watch the entire "Syria Undercover" piece at FRONTLINE's website.
16 November 2011
Double vision
The patient was impoverished and had been in and out of jail for years. His health was poor, and among our many worrying clinical findings was the possibility of undiagnosed advanced colon cancer.
A fellow med student and I spent almost an hour taking the patient's history. We noticed that many of the patient's problems had started two years ago. A fall two years ago had caused his left eye to permanently deviate outwards ("acquired exophoria"). No one had ever treated it, and he had been seeing double ("diplopia") ever since. Later on, he told us the story of how, two years ago, he went for a drive even though he wasn't supposed to. Just across the street from where he started his car, he crashed at full speed into a parked vehicle. The crash badly fractured his hip, altered his gait, and sent him to prison. He hadn't driven since.
The patient had communicated something important here that I had entirely missed.
My med school class just had a lecture about the eye, and I mentioned to a professor that I had recently examined a patient with diplopia and acquired exophoria. The professor replied that diplopia is very serious and, if uncorrected as in this patient, can thoroughly mess up someone's life. He said we should have made it our priority to identify the underlying cause and come up with a treatment plan. "You can't do much while seeing double," he said.
It was only then that I put two and two together: you can't drive a car while seeing double, either. The diplopia almost certainly caused the car crash, which caused the hip fractures, which wrecked his gait and caused him constant pain. Dominoes.
I've only just begun getting an intuition for which medical problems are most pressing. As it improves, I'll be able to do better for my patients.
A fellow med student and I spent almost an hour taking the patient's history. We noticed that many of the patient's problems had started two years ago. A fall two years ago had caused his left eye to permanently deviate outwards ("acquired exophoria"). No one had ever treated it, and he had been seeing double ("diplopia") ever since. Later on, he told us the story of how, two years ago, he went for a drive even though he wasn't supposed to. Just across the street from where he started his car, he crashed at full speed into a parked vehicle. The crash badly fractured his hip, altered his gait, and sent him to prison. He hadn't driven since.
The patient had communicated something important here that I had entirely missed.
My med school class just had a lecture about the eye, and I mentioned to a professor that I had recently examined a patient with diplopia and acquired exophoria. The professor replied that diplopia is very serious and, if uncorrected as in this patient, can thoroughly mess up someone's life. He said we should have made it our priority to identify the underlying cause and come up with a treatment plan. "You can't do much while seeing double," he said.
It was only then that I put two and two together: you can't drive a car while seeing double, either. The diplopia almost certainly caused the car crash, which caused the hip fractures, which wrecked his gait and caused him constant pain. Dominoes.
I've only just begun getting an intuition for which medical problems are most pressing. As it improves, I'll be able to do better for my patients.
10 November 2011
Safety net
Imagine: you're at an interview for a residency program. It's your fourth and final year at an accredited allopathic medical school in the United States. You listen to a voice mail from a classmate: your school has lost just its accreditation and the accrediting body says the decision is final. Effective immediately, you are ineligible for any American residency program. Unless you miraculously find another medical school that is willing to admit you and grant you advanced status, you will either have to start medical school over or find a new career. Your hundreds of thousands of dollars in loans are still due.
This account is not fiction. On October 3, 2011, the Liaison Committee on Medical Education (LCME), the accrediting body for allopathic medical schools in the U.S. and Canada, revoked the accreditation of San Juan Bautista School of Medicine because of "inadequate clinical resources". Although the school's administration knew that it was in danger of losing its accreditation, it had kept its students in the dark until the bitter end. The school enrolled 65 students in each class year.
A couple of schools are accepting a small number of San Juan Bautista students, but the majority of students appear to be absolutely out of luck.
It concerns me that not every medical students makes it. A fraction of those who enter medical school end up unable to practice medicine and saddled with a crushing load of debt. As the sizes of medical school classes increase nationwide and the number of residency spots remains the same, more students (especially those from studying at schools in the Caribbean) will find themselves stuck.
I wish there was a safety net. I'm not sure what it would be, but just some reassurance that if medicine doesn't work out, there's another viable career path that allows a student to pay off his debts.
As I go farther in medical school, I am increasingly committed to the profession. With that, I am increasingly entrusting some of my well-being to things beyond my control. All I can do is work to succeed and hope that everything turns out for the best.
UPDATE: The school's accreditation has been temporarily reinstated per a federal court injunction. Its fate remains in limbo.
This account is not fiction. On October 3, 2011, the Liaison Committee on Medical Education (LCME), the accrediting body for allopathic medical schools in the U.S. and Canada, revoked the accreditation of San Juan Bautista School of Medicine because of "inadequate clinical resources". Although the school's administration knew that it was in danger of losing its accreditation, it had kept its students in the dark until the bitter end. The school enrolled 65 students in each class year.
A couple of schools are accepting a small number of San Juan Bautista students, but the majority of students appear to be absolutely out of luck.
It concerns me that not every medical students makes it. A fraction of those who enter medical school end up unable to practice medicine and saddled with a crushing load of debt. As the sizes of medical school classes increase nationwide and the number of residency spots remains the same, more students (especially those from studying at schools in the Caribbean) will find themselves stuck.
I wish there was a safety net. I'm not sure what it would be, but just some reassurance that if medicine doesn't work out, there's another viable career path that allows a student to pay off his debts.
As I go farther in medical school, I am increasingly committed to the profession. With that, I am increasingly entrusting some of my well-being to things beyond my control. All I can do is work to succeed and hope that everything turns out for the best.
UPDATE: The school's accreditation has been temporarily reinstated per a federal court injunction. Its fate remains in limbo.
06 November 2011
MMI, oh my
Some medical schools have altered their admissions process by replacing the traditional applicant interview with the Multiple-Mini Interview (MMI). MMI resembles speed-dating: applicants rotate through numerous interview stations, where they act out scenarios and solve puzzles, sometimes alone and sometimes in groups. A July New York Times article presented a good overview of MMI, as implemented by Virginia Tech Carillon.
As you might expect, schools that have adopted MMI (UCLA and UC Davis among them) maintain its superiority to the traditional interview. For example, Stanford administrators praised the school's MMI program in a recent editorial:
I've interviewed under both formats. While I see strengths in both, I see many reasons why it would be a mistake for MMI to entirely replace the traditional interview:
In sum, I'm not convinced that MMI ought to replace traditional interviews. MMI's utility is unproven. Should more schools adopt MMI, I would expect students to adapt by obtaining schools' questions ahead of time and by practicing their acting skills. Lastly, because MMI does not evaluate an interviewee in the context of his application, it offers additional temptation to embellish one's qualifications.
MMI might be a great supplement to the traditional application process, but it strikes me as a poor replacement.
As you might expect, schools that have adopted MMI (UCLA and UC Davis among them) maintain its superiority to the traditional interview. For example, Stanford administrators praised the school's MMI program in a recent editorial:
Considering that as future physicians, candidates for medical school admission will be interacting with patients with diverse personalities and communication styles, we believe that it is essential to identify those skilled at interacting with multiple types of communicators...Scenarios are designed to probe candidates' ability to reason; to describe and support a particular point of view; or to analyze and discuss an ethical dilemma. There are no "right answers"; the effective communication of critical thinking skills is of the essence.
I've interviewed under both formats. While I see strengths in both, I see many reasons why it would be a mistake for MMI to entirely replace the traditional interview:
- Only the traditional interview deters applicants from embellishing their credentials.
Interviewers often try to confirm that elements of an application are truthful: if an applicant claims fluency in Spanish, an interviewer might introduce himself in Spanish. And for good reason--there is clear evidence that some medical students cheat. For example, researchers at Brigham & Women's Hospital established that at least 1 in 20 applicants to their most competitive residency programs had plagiarized their personal statements. MMI refuses to evaluate applicants in the context of their application, a huge drawback that encourages cheating.
- MMI questions can be found out ahead of time, and MMI can probably be coached.
Many schools purchase a bank of MMI questions from McMaster University in Canada and reuse their questions day to day and year to year. Some schools request that interviewees sign non-disclosure agreements (NDAs) to keep the MMI scenarios they witness a secret. Not all applicants abide by the NDAs and a well-connected student would have little trouble finding out the questions. For that matter, a publicly available fact-sheet put out by McMaster lays out two of the MMI scenarios that I encountered on the interview trail.
My impression is that MMIs are coachable: most of the stations involved extemporaneous acting, and having taken improvisational acting as an undergraduate was a tremendous help. After all, if MMI weren't coachable, why would schools need interviewees to sign NDAs? I've already noticed that colleges are putting on "mock MMIs" for their pre-meds. The coachability of MMI will increasingly limit its ability to objectively evaluate interviewees. - The main research studies on MMI are not as relevant as they might appear.
The main studies on MMI come from McMaster University (the school that profits by licensing MMI questions, which strikes me as a substantial conflict-of-interest). Researchers asked applicants undergoing traditional interviews to volunteer to participate in a trial MMI. Neither the student's performance in the MMI nor his decision whether to participate would be considered in the admissions process. The study looked within this sample of volunteers and found that higher scores on the MMI moderately correlated with better evaluations on clinical clerkships. Universities cite this study as evidence that MMI ought to replace the traditional interview.
The fallacy in citing this study is that it only examined applicants who performed well enough on the traditional interview to be admitted. The study does not tell us that MMI by itself is better than a traditional interview at assessing candidates. Rather, it suggests that succeeding on both correlates more strongly to good clerkship evaluations than does succeeding on the traditional interview alone. It's not clear that MMI alone is any better than the traditional interview, and indeed, MMI alone may be much worse. The study is analogous to my asking, "of the girls who I would have an excellent time with on a long date (traditional interview), does how much I enjoy talking to them at a cocktail party (MMI) correlate to how good of a couple we would make?" Even if the answer is yes, it doesn't mean that when I seek out mates I should abandon dates and only attend cocktail parties.
I agree with the Stanford administrators that the traditional interview and MMI test different skill sets: the interview requires depth and is a one-on-one exploration of someone's person and character; the MMI assesses how well someone communicates and improvises in different situations. It makes sense that the best doctors have both of these skills, but I have not seen evidence that one set of skills is better than the other.
In sum, I'm not convinced that MMI ought to replace traditional interviews. MMI's utility is unproven. Should more schools adopt MMI, I would expect students to adapt by obtaining schools' questions ahead of time and by practicing their acting skills. Lastly, because MMI does not evaluate an interviewee in the context of his application, it offers additional temptation to embellish one's qualifications.
MMI might be a great supplement to the traditional application process, but it strikes me as a poor replacement.
31 October 2011
Power of deduction
One professor told us that entering the medical profession would make people see us differently. Another told us the corollary: that entering the medical profession would make us see people differently. I can already feel it happening.
Twice today I noticed a person whose gait was abnormal. Automatically I tried to classify the abnormality and predict what underlying disease it might signify.
Twice today I noticed a person whose gait was abnormal. Automatically I tried to classify the abnormality and predict what underlying disease it might signify.
26 October 2011
Time remaining
The milestone of the world's population reaching 7 billion is a fitting time to reflect upon life expectancy. Life expectancy is a rough marker of humanity and medicine's progress in the age-old battle to attain old age.
Those born in the US this year are expected to live until 78.37 years of age if current mortality rates persist. This puts us at a sobering 50th in the world.
How long is someone your age expected to live? It's tempting, but erroneous, to calculate it as follows:
Knowing how long a patient has to live can inform treatment options. The use of CT scans in children is kept to minimum, because the high levels of radiation can induce secondary tumors decades later. On the other hand, patients with terminal cancer sometimes undergo radiation therapy to relieve pain--their current cancer will prove fatal long before a cancer induced by the radiation. A patient's estimated remaining number of years are factored into screening guidelines for breast and prostate cancer.
This increasing reliance on life expectancy brings up all kinds of fascinating ethical conundrums. If too many medical decisions become centered around life expectancy, life expectancy could become a self-fulfilling prophecy and an entrenched form of discrimination. Should a teenage male needing a kidney should get preference over an elderly woman, simply because he is expected to live longer? If so, should an African-American person get a kidney before a Native American? Should a richer person get a kidney before a poorer person? What about people with life-shortening diseases that hit certain ethnic groups more frequently (sickle-cell anemia, Huntington Disease, Gaucher disease, cystic fibrosis)?
Seeing how life expectancy changes over time gives us a sense of how far we have come, largely thanks to advances in nutrition, sanitation, and combating infectious disease. In 1850, US life expectancy at birth was 38 years, just under half what it is now. 38 years is also the current life expectancy of someone born in AIDS-ravaged Angola.
Why is the US life expectancy so low relative to other industrialized countries', especially when our politicians claim we have the greatest medical system in the world? Monaco's is 90! Main contributors are our obesity rate and smoking rate, or put another way, our government's lack of emphasis on public health. Low-hanging fruit would include increasing cigarette taxes (which significantly decrease smoking rates) and tackling our burgeoning obesity problem.
78.37 years is a simple number with immense ramifications.
Those born in the US this year are expected to live until 78.37 years of age if current mortality rates persist. This puts us at a sobering 50th in the world.
How long is someone your age expected to live? It's tempting, but erroneous, to calculate it as follows:
Current life expectancy - my current age = my expected remaining yearsWhy? For one, your overall life expectancy increases as you grow older; lumped into the life expectancy figure were those who died in infancy and childhood. A 30 year-old today is expected to live until 81.5 years; a 65 year-old until age 85. The key resource here is an actuarial life table, such as this one published by the Social Security Administration. More detailed actuarial estimates will take into account your family history; your medical history; your smoking, eating, and drinking habits; your weight; and your education level; all of which contribute substantially.
Knowing how long a patient has to live can inform treatment options. The use of CT scans in children is kept to minimum, because the high levels of radiation can induce secondary tumors decades later. On the other hand, patients with terminal cancer sometimes undergo radiation therapy to relieve pain--their current cancer will prove fatal long before a cancer induced by the radiation. A patient's estimated remaining number of years are factored into screening guidelines for breast and prostate cancer.
This increasing reliance on life expectancy brings up all kinds of fascinating ethical conundrums. If too many medical decisions become centered around life expectancy, life expectancy could become a self-fulfilling prophecy and an entrenched form of discrimination. Should a teenage male needing a kidney should get preference over an elderly woman, simply because he is expected to live longer? If so, should an African-American person get a kidney before a Native American? Should a richer person get a kidney before a poorer person? What about people with life-shortening diseases that hit certain ethnic groups more frequently (sickle-cell anemia, Huntington Disease, Gaucher disease, cystic fibrosis)?
Seeing how life expectancy changes over time gives us a sense of how far we have come, largely thanks to advances in nutrition, sanitation, and combating infectious disease. In 1850, US life expectancy at birth was 38 years, just under half what it is now. 38 years is also the current life expectancy of someone born in AIDS-ravaged Angola.
Why is the US life expectancy so low relative to other industrialized countries', especially when our politicians claim we have the greatest medical system in the world? Monaco's is 90! Main contributors are our obesity rate and smoking rate, or put another way, our government's lack of emphasis on public health. Low-hanging fruit would include increasing cigarette taxes (which significantly decrease smoking rates) and tackling our burgeoning obesity problem.
78.37 years is a simple number with immense ramifications.
25 October 2011
One glance
Four classmates and I were swapping stories at our table in a restaurant, unwinding after a major exam. One of us was still in his scrubs, and our waiter, overhearing our conversation, asked if we were medical students. When we responded in the affirmative, he told us that his mother recently had been diagnosed with a brain tumor and had to get it surgically removed. "It was so stressful waiting for the neurosurgeon to come into the waiting room and tell me and my dad how the procedure turned out," he told us.
"Finally, he came out, and his face was a total blank. Absolutely no expression. Couldn't read anything. I guess that's what he has to do, but those fifteen seconds when the surgeon walked over felt like an hour. With each step he took I kept feeling like something must have gone wrong, my mom must be dead.
"Then he pulled my father aside, and said that everything went great. I was so mad at him that I wanted to punch him, but I was so happy about what he said that I wanted to dance. I can't believe what that guy put me through."
Our once-boisterous table was silent.
Some weeks back, a professor had told us that practicing medicine is a privilege and a burden--you can restore life or take it away, and with one glance or a few words you can alter someone's life, for better or for worse. He told us that people will treat us differently and expect more of us, just because we are medical students and someday, physicians.
Our waiter just wanted to tell us his story. And without knowing it, he had reminded us that our professor was right.
"Finally, he came out, and his face was a total blank. Absolutely no expression. Couldn't read anything. I guess that's what he has to do, but those fifteen seconds when the surgeon walked over felt like an hour. With each step he took I kept feeling like something must have gone wrong, my mom must be dead.
"Then he pulled my father aside, and said that everything went great. I was so mad at him that I wanted to punch him, but I was so happy about what he said that I wanted to dance. I can't believe what that guy put me through."
Our once-boisterous table was silent.
Some weeks back, a professor had told us that practicing medicine is a privilege and a burden--you can restore life or take it away, and with one glance or a few words you can alter someone's life, for better or for worse. He told us that people will treat us differently and expect more of us, just because we are medical students and someday, physicians.
Our waiter just wanted to tell us his story. And without knowing it, he had reminded us that our professor was right.
24 October 2011
Misbehavior
The ongoing Conrad Murray trial has introduced the public to one of medicine's underworlds--those doctors who break laws and abuse the status and privileges conferred by their profession.
I occasionally read state medical licensing boards' write-ups of disciplinary actions, and some read like crime thrillers. One case report abhorred me. A New York general surgeon had an affair with a married patient just after performing her hysterectomy (removal of the uterus). What made the case particularly sinister was the abuse of the doctor-patient relationship. The surgeon repeatedly phoned the patient requesting that she return to clinic for post-operative follow-up (generally, office staff place these types of phone calls). He had her come in after-hours, when office staff weren't around. When the patient revealed her worry that her husband might no longer find her attractive, the surgeon replied that he personally found her beautiful and kissed her on the lips. An affair developed, the surgeon's insistent overtures leading to a nighttime liaison at a motel. Patients with hysterectomies are supposed to wait a certain number of weeks before engaging in conjugal relations, and the surgeon damaged the patient's stitching.
The medical board investigation found that the surgeon also had badly botched at least two patients' surgeries and had made inappropriate sexual advances on at least two other female patients. Its condemnation was harsh:
The board revoked the surgeon's license, its most severe punishment. I doubt the surgeon's wife was pleased. I couldn't find a record of criminal charges being brought against him, and it's not clear to me what he could have been charged with.
Yet there was also a hero of sorts: the patient's primary-care doctor. During a routine office visit with the patient he intuited that something was wrong. He asked around and gathered from another patient that the surgeon was behaving inappropriately. He brought the matter to the attention of the state board.
Plenty of violations result in reprimands, probationary licenses, restricted licenses, suspension, and for the most egregious misdeeds, revocation. Doctors get rapped on the knuckles for failing to promptly inform the board of a DUI conviction, or for repeatedly botching surgeries in ways that should have been avoided, or for keeping poor notes. Although policies vary state to state, looking up a physician's record used to be expensive and slow. Now, most states provide these records on-line, free of charge. I think the trend is on the whole a good one. Patients ought to know who they are entrusting their care to.
There is plenty more to discuss here. The medical board system resembles the criminal system: it is punitive, reactionary, and slow. There isn't a good infrastructure to help physicians whose performance is slipping (for example, a surgeon who is losing dexterity). And there aren't many jobs doctors can do besides medicine, meaning doctors who ought to hang up their stethoscope, and want to, might not be able to.
We need to discipline doctors who violate the rules. Yet we also need to set up a system that makes it easier to identify at-risk physicians and get them help, before the state medical board has to take their license away.
I occasionally read state medical licensing boards' write-ups of disciplinary actions, and some read like crime thrillers. One case report abhorred me. A New York general surgeon had an affair with a married patient just after performing her hysterectomy (removal of the uterus). What made the case particularly sinister was the abuse of the doctor-patient relationship. The surgeon repeatedly phoned the patient requesting that she return to clinic for post-operative follow-up (generally, office staff place these types of phone calls). He had her come in after-hours, when office staff weren't around. When the patient revealed her worry that her husband might no longer find her attractive, the surgeon replied that he personally found her beautiful and kissed her on the lips. An affair developed, the surgeon's insistent overtures leading to a nighttime liaison at a motel. Patients with hysterectomies are supposed to wait a certain number of weeks before engaging in conjugal relations, and the surgeon damaged the patient's stitching.
The medical board investigation found that the surgeon also had badly botched at least two patients' surgeries and had made inappropriate sexual advances on at least two other female patients. Its condemnation was harsh:
Respondent has shown himself to be morally bankrupt...[He] used his status as a physician as a tool to obtain personal gratification from women who were his patients. In perverting his standing as a physician, Respondent did not only have a negative effect on the individual patients, he disrupted entire families.Furthermore, as the facts in this matter become known, first to colleagues and ultimately to the community as a whole, Respondent has hurt his entire profession. Each time a physician betrays the trust bestowed upon him by virtue of his status as a license holder, the public has a right to take notice and wonder at the trustworthiness of all practitioners.
Yet there was also a hero of sorts: the patient's primary-care doctor. During a routine office visit with the patient he intuited that something was wrong. He asked around and gathered from another patient that the surgeon was behaving inappropriately. He brought the matter to the attention of the state board.
Plenty of violations result in reprimands, probationary licenses, restricted licenses, suspension, and for the most egregious misdeeds, revocation. Doctors get rapped on the knuckles for failing to promptly inform the board of a DUI conviction, or for repeatedly botching surgeries in ways that should have been avoided, or for keeping poor notes. Although policies vary state to state, looking up a physician's record used to be expensive and slow. Now, most states provide these records on-line, free of charge. I think the trend is on the whole a good one. Patients ought to know who they are entrusting their care to.
There is plenty more to discuss here. The medical board system resembles the criminal system: it is punitive, reactionary, and slow. There isn't a good infrastructure to help physicians whose performance is slipping (for example, a surgeon who is losing dexterity). And there aren't many jobs doctors can do besides medicine, meaning doctors who ought to hang up their stethoscope, and want to, might not be able to.
We need to discipline doctors who violate the rules. Yet we also need to set up a system that makes it easier to identify at-risk physicians and get them help, before the state medical board has to take their license away.
23 October 2011
Who is a doctor, anyway?
As an undergrad I bristled at lecturers' (non-faculty instructors) being referred to as "Professor". I don't believe a title should be used until it's earned. Yet as a student who sometimes examines patients, I'm occasionally referred to as "Doctor" (sometimes by patients, sometimes by physicians). I shy away from the title, although I feel uncomfortable correcting an attending physician in front of a patient. That said, students sometimes try out the title as though trying on a spiffy business suit, incorporating "Dr." into their e-mail addresses and blogs or addressing classmates in jest as "Doctor."
Lots of people are clamoring to be called "Doctor", and a recent New York Times article focuses on some nurse practitioners' push to be called "Doctor" in a clinical setting. Nurse practitioners now have to earn a DNP, a clinically-oriented doctoral-level degree (although it often entails three years of training beyond a bachelors', which would make many Ph.D. students green with envy). The subject of the article is a nurse who introduces herself thusly to patients: "Hi. I’m Dr. Patti McCarver, and I’m your nurse."
I believe Nurse McCarver errs in using the title of "Doctor" in a clinical setting.
First, an analogy. A classmate entered medical school with a doctorate in Romance languages. During our third-year rotations, could he rightfully introduce himself as "Doctor" to a patient? Absolutely not. It's confusing at best and disingenuous at worst. Yet, if the Ph. D. shouldn't be called "Doctor" in front of patients, why should a DNP?
Also, if most health-care providers were to refer to themselves the same way, wouldn't the title lose some of its ability to convey useful information in a health-care setting?
Physicians, optometrists, dentists, podiatrists, and some psychologists can unquestionably call themselves "doctor" when interacting with human patients. I fail to see the need to include some types of nurses as well.
State legislatures have entered the fray, with a handful of states explicitly awarding nurse practitioners the title and a handful expressly forbidding it. So long as this turf war wears on, there will be no shortage of confused patients.
Lots of people are clamoring to be called "Doctor", and a recent New York Times article focuses on some nurse practitioners' push to be called "Doctor" in a clinical setting. Nurse practitioners now have to earn a DNP, a clinically-oriented doctoral-level degree (although it often entails three years of training beyond a bachelors', which would make many Ph.D. students green with envy). The subject of the article is a nurse who introduces herself thusly to patients: "Hi. I’m Dr. Patti McCarver, and I’m your nurse."
I believe Nurse McCarver errs in using the title of "Doctor" in a clinical setting.
First, an analogy. A classmate entered medical school with a doctorate in Romance languages. During our third-year rotations, could he rightfully introduce himself as "Doctor" to a patient? Absolutely not. It's confusing at best and disingenuous at worst. Yet, if the Ph. D. shouldn't be called "Doctor" in front of patients, why should a DNP?
Also, if most health-care providers were to refer to themselves the same way, wouldn't the title lose some of its ability to convey useful information in a health-care setting?
Physicians, optometrists, dentists, podiatrists, and some psychologists can unquestionably call themselves "doctor" when interacting with human patients. I fail to see the need to include some types of nurses as well.
State legislatures have entered the fray, with a handful of states explicitly awarding nurse practitioners the title and a handful expressly forbidding it. So long as this turf war wears on, there will be no shortage of confused patients.
21 October 2011
A walk through the valley of the shadow of death
"Medical student syndrome" is a mainstay of medical training: many students become convinced that they or those around them are experiencing the symptoms of some of the diseases they study. I don't feel like I am suffering from the syndrome, but learning the sheer variety of diseases has made me more frightened of succumbing to one. I had been blissfully ignorant of most of the myriad ways our extraordinarily complex body fails. I now find myself worrying more about aging and about those I love falling ill.
Becoming acquainted with death and its pernicious relations is part of the burden and privilege of medical training. Soon we will be assuming shared responsibility for our patients' well-being, and we must know their enemies to best protect against them.
Fretting that things might be more serious than they appear can be a mark of a good physician. If a teenage patient breaks his femur while playing football, it's one thing to repair the leg and cast it. It's rather another to step back and wonder if the bone had broken because it was weakened (perhaps by cancer or an endocrine disorder). Seemingly innocuous complaints (muscle twitches in the leg) can have unlikely but serious conditions in their differential diagnosis (amyotrophic lateral sclerosis, aka Lou Gehrig's disease). This decision of whether to pursue a case further is informed by years of experience, something I currently lack.
I was taught that one needs to feel concern in moderation; too much worry is disabling and too little is reckless. I hope to strike the right balance, for my sake and for my patients'.
Becoming acquainted with death and its pernicious relations is part of the burden and privilege of medical training. Soon we will be assuming shared responsibility for our patients' well-being, and we must know their enemies to best protect against them.
Fretting that things might be more serious than they appear can be a mark of a good physician. If a teenage patient breaks his femur while playing football, it's one thing to repair the leg and cast it. It's rather another to step back and wonder if the bone had broken because it was weakened (perhaps by cancer or an endocrine disorder). Seemingly innocuous complaints (muscle twitches in the leg) can have unlikely but serious conditions in their differential diagnosis (amyotrophic lateral sclerosis, aka Lou Gehrig's disease). This decision of whether to pursue a case further is informed by years of experience, something I currently lack.
I was taught that one needs to feel concern in moderation; too much worry is disabling and too little is reckless. I hope to strike the right balance, for my sake and for my patients'.
15 October 2011
Responding to mass-casualty plane crashes
It heartens me to see the medical community's tremendous response to extraordinarily demanding disasters. The Reno airshow crash this September sent 35 patients, many of them grievously wounded from complex trauma, to a particular hospital's emergency department. Reno's main newspaper described the situation inside the ED in a riveting article.
The ED began preparing for patients as soon as they received word of the crash, and an automated telephone system requested that off-duty emergency medicine physicians come in immediately. Physicians from all types of specialties flocked to the hospital unasked so that they could be on-hand. What resulted was remarkably efficient and collaborative care.
I'm reminded also of the 1989 crash of United Flight 232 in Sioux City, IA. 296 people were aboard the DC-10, which due to improper maintenance lost its tail engine and all of its hydraulics. This meant no flight controls (throttle, rudder, elevators, ailerons), no landing gear, and no brakes. All that the pilots could control was the amount of fuel going to their two remaining engines. By opening and cutting off the fuel lines, the pilots were able to very crudely control their altitude and somewhat guide the plane, which was constantly turning right. Through a combination of sheer luck, skill, experience, and the assistance of a quick-thinking air traffic controller, the pilots guided the plane over Sioux Falls airport and crash-landed near the runway.
Approximately 200 survivors were rushed to Sioux City's hospital. Physicians, in turn, rushed in to help assist. There were so many physicians on hand that the hospital director arranged for each arriving patient to be met by a team of a doctor, a nurse, and a technician. This team would remain with the patient until they were either discharged from the hospital or admitted. Miraculously, 185 aboard the plane lived.
Sioux City had conducted a mass-casualty simulation a little over a year prior to prepare its emergency response services. The scenario: a passenger aircraft crash-landing at Sioux City airport.
Tragedies can sometimes bring out the best in people, and in these tragic crashes the medical community put its best foot forward.
The ED began preparing for patients as soon as they received word of the crash, and an automated telephone system requested that off-duty emergency medicine physicians come in immediately. Physicians from all types of specialties flocked to the hospital unasked so that they could be on-hand. What resulted was remarkably efficient and collaborative care.
I'm reminded also of the 1989 crash of United Flight 232 in Sioux City, IA. 296 people were aboard the DC-10, which due to improper maintenance lost its tail engine and all of its hydraulics. This meant no flight controls (throttle, rudder, elevators, ailerons), no landing gear, and no brakes. All that the pilots could control was the amount of fuel going to their two remaining engines. By opening and cutting off the fuel lines, the pilots were able to very crudely control their altitude and somewhat guide the plane, which was constantly turning right. Through a combination of sheer luck, skill, experience, and the assistance of a quick-thinking air traffic controller, the pilots guided the plane over Sioux Falls airport and crash-landed near the runway.
Approximately 200 survivors were rushed to Sioux City's hospital. Physicians, in turn, rushed in to help assist. There were so many physicians on hand that the hospital director arranged for each arriving patient to be met by a team of a doctor, a nurse, and a technician. This team would remain with the patient until they were either discharged from the hospital or admitted. Miraculously, 185 aboard the plane lived.
Sioux City had conducted a mass-casualty simulation a little over a year prior to prepare its emergency response services. The scenario: a passenger aircraft crash-landing at Sioux City airport.
Tragedies can sometimes bring out the best in people, and in these tragic crashes the medical community put its best foot forward.
12 October 2011
Procrustes
The wisdom of the ancient Greeks can still inform modern medical practice.
In mythology, Procrustes was a mischievous innkeeper who offered every traveler a bed. However, the bed was made of iron, and he would either stretch the travelers out or amputate their legs to make them fit perfectly. In one version, Procrustes kept two different-sized beds to ensure that no one fit. The Athenian hero Theseus killed Procrustes, ending his reign of terror.
An excellent contemporary book on physical diagnosis, Sapira's, advises how to ask the patient good questions about their history. It warns against having preconceived notions of the patient's diagnosis and forcing the patient's story to conform to it, calling such practitioners "Procrusteans."
In mythology, Procrustes was a mischievous innkeeper who offered every traveler a bed. However, the bed was made of iron, and he would either stretch the travelers out or amputate their legs to make them fit perfectly. In one version, Procrustes kept two different-sized beds to ensure that no one fit. The Athenian hero Theseus killed Procrustes, ending his reign of terror.
An excellent contemporary book on physical diagnosis, Sapira's, advises how to ask the patient good questions about their history. It warns against having preconceived notions of the patient's diagnosis and forcing the patient's story to conform to it, calling such practitioners "Procrusteans."
Doctor Hotspot
The most expensive place in the hospital to receive health care is in the Emergency Department. Federal laws mandate that hospitals treat critically ill patients regardless of their ability to pay, leaving taxpayers to foot the bill.
A pioneering family practitioner, Dr. Jeffrey Brenner, found that a small handful of patients in his city of Camden, NJ were responsible for a disproportionate share of ER costs. He decided to provide those patients with primary care, keeping them out of the hospital, with substantial savings to the public. Among his innovations are including "health coaches" on his medical staff, who befriend and encourage the patients to follow their health regimens.
FRONTLINE, my favorite TV program, teamed up with Dr. Atul Gawande, my favorite medical writer, for this 15-minute documentary on Brenner's work.
Gawande also wrote a longer piece for the New Yorker last year.
Dr. Brenner's model is exciting because it highlights the likely strengths of a robust primary-care system: cost savings and better health.
A pioneering family practitioner, Dr. Jeffrey Brenner, found that a small handful of patients in his city of Camden, NJ were responsible for a disproportionate share of ER costs. He decided to provide those patients with primary care, keeping them out of the hospital, with substantial savings to the public. Among his innovations are including "health coaches" on his medical staff, who befriend and encourage the patients to follow their health regimens.
FRONTLINE, my favorite TV program, teamed up with Dr. Atul Gawande, my favorite medical writer, for this 15-minute documentary on Brenner's work.
Watch Doctor Hotspot on PBS. See more from FRONTLINE.
Gawande also wrote a longer piece for the New Yorker last year.
Dr. Brenner's model is exciting because it highlights the likely strengths of a robust primary-care system: cost savings and better health.
27 September 2011
Mistakes
My heart sank and I swallowed nervously. I had just finished administering a vaccine for the second time ever, and the syringe's plunger felt strange as I finished pushing it in. It hit me. I had forgotten to check the vaccine for air bubbles, and I had injected a bit of air into my patient's left deltoid. I pictured him climbing into bed that night and dying of an air embolism, a cruel fate brought on by a vaccine that was supposed to protect from harm.
I tried to look calm and found an attending physician, who assured me that everything was fine. The amount of air in vaccines is miniscule, and in fact, having a bit of air in the syringe often helps an intramuscular injection. No harm done. But I was still shaken. Just like that, I had skipped a step that I had believed at the time to be critical.
The experience convinced me of just how easy it is to commit a medical error.
Even a simple procedure like administering a vaccine involves a number of important sequential steps. The sharps disposal container needs to be placed within arm's reach before the needle's cap is removed. The medical chart needs to be double-checked to ensure that the correct vaccination is being given. The injection site needs to be disinfected properly. Inevitably, even the best practitioners mess up a step. Medical errors are a tremendous problem, responsible for 48,000 to 98,000 deaths per year.
There is a growing movement to use checklists when carrying out medical procedures, just as pilots do when they fly. My favorite medical writer, Prof. Atul Gawande, wrote a fascinating article in the New Yorker on the subject, which I encourage you to read for free. Yes, individuals commit errors, yet the systems they work in can reduce the likelihood of those errors. For example, anesthesiology equipment wasn't standardized in the past, and turning a knob to the right would release more anesthetic on some machines and release less anesthetic on others. Now the equipment is consistent at every hospital in the country, avoiding needless deaths.
The fruits of prevention efforts are masked. When a hospital implements a labeling system to avoid wrong-side surgeries, patients who are saved won't know how narrowly they avoided catastrophe. It's not very obvious when the system succeeds, only when it fails. But even if prevention isn't sexy, we need to still try. Avoiding medical errors is inexpensive, it saves lives, and it is the right thing to do. For my part, I'm writing up a checklist for myself on how to administer vaccines properly.
Photo reproduced with permission via Creative Commons license. Author: @alviseni
I tried to look calm and found an attending physician, who assured me that everything was fine. The amount of air in vaccines is miniscule, and in fact, having a bit of air in the syringe often helps an intramuscular injection. No harm done. But I was still shaken. Just like that, I had skipped a step that I had believed at the time to be critical.
The experience convinced me of just how easy it is to commit a medical error.
Even a simple procedure like administering a vaccine involves a number of important sequential steps. The sharps disposal container needs to be placed within arm's reach before the needle's cap is removed. The medical chart needs to be double-checked to ensure that the correct vaccination is being given. The injection site needs to be disinfected properly. Inevitably, even the best practitioners mess up a step. Medical errors are a tremendous problem, responsible for 48,000 to 98,000 deaths per year.
There is a growing movement to use checklists when carrying out medical procedures, just as pilots do when they fly. My favorite medical writer, Prof. Atul Gawande, wrote a fascinating article in the New Yorker on the subject, which I encourage you to read for free. Yes, individuals commit errors, yet the systems they work in can reduce the likelihood of those errors. For example, anesthesiology equipment wasn't standardized in the past, and turning a knob to the right would release more anesthetic on some machines and release less anesthetic on others. Now the equipment is consistent at every hospital in the country, avoiding needless deaths.
The fruits of prevention efforts are masked. When a hospital implements a labeling system to avoid wrong-side surgeries, patients who are saved won't know how narrowly they avoided catastrophe. It's not very obvious when the system succeeds, only when it fails. But even if prevention isn't sexy, we need to still try. Avoiding medical errors is inexpensive, it saves lives, and it is the right thing to do. For my part, I'm writing up a checklist for myself on how to administer vaccines properly.
Photo reproduced with permission via Creative Commons license. Author: @alviseni
26 September 2011
An afternoon at elementary school
How familiar are inner-city kids with vegetables and healthy eating? I was pleasantly surprised to find out.
A classmate arranged for interested students to design and deliver an hour-long presentation about health at an inner-city elementary school. I signed up and received my assignment: first graders. How can anyone spend an hour discussing medicine with kids who can't tie their own shoes?
Lost, I turned to my brother for help. He challenged me to do something about obesity, sending along this must-see (but probably heavily-edited) video from Jamie Oliver's Food Revolution. The first-graders shown live in one of the most obese counties in the nation:
A challenge took shape: could my first-graders outdo their Huntington, West Virginia counterparts in identifying vegetables? With little more than a white coat, stethoscope, and zealous enthusiasm, could I inspire young children to improve their diets? My brother proposed a curriculum:
1. Explain how vegetables are a delicious and awesome part of a balanced diet.
2. Show various vegetables and see if students can identify them.
3. Have students draw a picture that has a vegetable in it.
4. Have students vote for their favorite vegetable.
5. Explain that anyone can be a doctor if they work hard in all subjects in school.
6. Feast on baby carrots.
I woke up early to snag exactly one of every vegetable from the local food co-op. My trip to the check-out portended badly for the vegetable quiz later that day, when the clerk and I disagreed over whether a root vegetable in my basket should be rung up as a leek or a garlic stalk.
A thoughtful classmate who is passionate about nutrition and excellent with kids thankfully offered to join me and split teaching duties. We drove to a rough part of town and found our school.
First graders say adorable things. Our presentation began something like this:
Med Student A: "We're medical students and we're here today to talk about vegetables! Vegetables are...yes, I see a hand."
Ashley: "One time, I got sick and I throwed up."
Med Student A: "Yes, that happens sometimes. Another question?"
Josiah: "My throat hurted...and...my dad made me eat ice."
Med Student B: "Yes! Ice can be good for you. So, about vegetables--"
Deidre: "I ate a banana yesterday for dinner."
Med Student B: "Awesome! I love bananas too! They're so delicious and good for you! So vegetables are..."
We eventually moved on to the quiz. Students successfully identified broccoli, carrots, cucumbers, and even eggplant. They displayed a surprisingly good grasp of what sorts of food were nutritious and which were not. They understood where vegetables grow, where they can be purchased, and even that you can grow your own vegetables in your garden and your yard. Our election crowned carrots as the crowd favorite, although ballot-stuffing plagued the polls. Unfortunately, "one man, one vote" is so foreign a concept that we tallied 50 votes among only 20 students. Fortunately, their math skills were so elementary (15 minus 11 was beyond their powers) that no one realized the election was a sham.
The students unleashed their creative juices and were keen to show us their handiwork. We saw plenty of fruits and vegetables as well as a few head-scratchers.
Annalise (holding up drawing): "What is this?"
Me: "That looks like a bunch of grapes!"
Annalise: "And this?"
Me: "That's a beautiful banana!"
Annalise: "What is this?"
Me: "Umm...I'm not really sure what that is. Is that an airplane?"
Annalise: "Aero-plane!"
It felt like I was doing improv acting again, where I had to heartily embrace all of my fellow actors' ideas (even when it meant portraying a crazed edentulous Gulf Coast fisherman) and encourage and support them. These young minds were delightfully bursting with creativity and non sequiturs.
At the end, it was time to feast on baby carrots. I have never seen kids so excited to eat carrots before. Even the kids on the playground, who we didn't teach at all, devoured our carrots after my fellow med student and I gushed over how delicious they are. Saturday morning cartoons are filled with advertisements successfully pushing sugary cereals and candy onto these malleable young minds. But this one wonderful afternoon, vegetables reigned king.
In the fight against obesity, there is hope after all.
A classmate arranged for interested students to design and deliver an hour-long presentation about health at an inner-city elementary school. I signed up and received my assignment: first graders. How can anyone spend an hour discussing medicine with kids who can't tie their own shoes?
Lost, I turned to my brother for help. He challenged me to do something about obesity, sending along this must-see (but probably heavily-edited) video from Jamie Oliver's Food Revolution. The first-graders shown live in one of the most obese counties in the nation:
A challenge took shape: could my first-graders outdo their Huntington, West Virginia counterparts in identifying vegetables? With little more than a white coat, stethoscope, and zealous enthusiasm, could I inspire young children to improve their diets? My brother proposed a curriculum:
1. Explain how vegetables are a delicious and awesome part of a balanced diet.
2. Show various vegetables and see if students can identify them.
3. Have students draw a picture that has a vegetable in it.
4. Have students vote for their favorite vegetable.
5. Explain that anyone can be a doctor if they work hard in all subjects in school.
6. Feast on baby carrots.
I woke up early to snag exactly one of every vegetable from the local food co-op. My trip to the check-out portended badly for the vegetable quiz later that day, when the clerk and I disagreed over whether a root vegetable in my basket should be rung up as a leek or a garlic stalk.
A thoughtful classmate who is passionate about nutrition and excellent with kids thankfully offered to join me and split teaching duties. We drove to a rough part of town and found our school.
First graders say adorable things. Our presentation began something like this:
Med Student A: "We're medical students and we're here today to talk about vegetables! Vegetables are...yes, I see a hand."
Ashley: "One time, I got sick and I throwed up."
Med Student A: "Yes, that happens sometimes. Another question?"
Josiah: "My throat hurted...and...my dad made me eat ice."
Med Student B: "Yes! Ice can be good for you. So, about vegetables--"
Deidre: "I ate a banana yesterday for dinner."
Med Student B: "Awesome! I love bananas too! They're so delicious and good for you! So vegetables are..."
We eventually moved on to the quiz. Students successfully identified broccoli, carrots, cucumbers, and even eggplant. They displayed a surprisingly good grasp of what sorts of food were nutritious and which were not. They understood where vegetables grow, where they can be purchased, and even that you can grow your own vegetables in your garden and your yard. Our election crowned carrots as the crowd favorite, although ballot-stuffing plagued the polls. Unfortunately, "one man, one vote" is so foreign a concept that we tallied 50 votes among only 20 students. Fortunately, their math skills were so elementary (15 minus 11 was beyond their powers) that no one realized the election was a sham.
 | |
| The election candidates |
The students unleashed their creative juices and were keen to show us their handiwork. We saw plenty of fruits and vegetables as well as a few head-scratchers.
Annalise (holding up drawing): "What is this?"
Me: "That looks like a bunch of grapes!"
Annalise: "And this?"
Me: "That's a beautiful banana!"
Annalise: "What is this?"
Me: "Umm...I'm not really sure what that is. Is that an airplane?"
Annalise: "Aero-plane!"
It felt like I was doing improv acting again, where I had to heartily embrace all of my fellow actors' ideas (even when it meant portraying a crazed edentulous Gulf Coast fisherman) and encourage and support them. These young minds were delightfully bursting with creativity and non sequiturs.
At the end, it was time to feast on baby carrots. I have never seen kids so excited to eat carrots before. Even the kids on the playground, who we didn't teach at all, devoured our carrots after my fellow med student and I gushed over how delicious they are. Saturday morning cartoons are filled with advertisements successfully pushing sugary cereals and candy onto these malleable young minds. But this one wonderful afternoon, vegetables reigned king.
In the fight against obesity, there is hope after all.
21 September 2011
The con man
Some of literature's most beloved characters thrive by cunningly misleading others (Odysseus, Don Juan, and Tom Sawyer come to mind). Yes, we scorn liars and con men, but we also celebrate those who have mastered the art of lies.
Some of the most befuddling and tragic "con men" a doctor will see are those with Munchausen syndrome, who intentionally exaggerate, induce, or simulate illness or injury, in order "to assume the sick role." Munchausen syndrome by proxy occurs when someone intentionally induces or simulates injury in another (typically their child).
Diagnosing a patient can sometimes be like answering a trick question: the ordinary rules don't always apply. A case report in the NEJM reads like a detective story. A healthy-seeming toddler presented to a clinic because of a "reported febrile convulsion." Blood samples were taken on several occasions and given to the patient's mother, who dropped them off at the laboratory for processing. Each one showed potassium and creatinine levels so high as to be "incompatible with life." This apparently piqued the interest of the physicians, who recognized that the readings were factitious (not reflective of reality).
The doctors readminstered the blood test and gave the mother two blood samples with her daughter's name on it--except that one secretly contained a different patient's blood whose lab values were known. Sure enough, both blood samples came back with impossibly high potassium and creatinine levels.
The physicians knew of another bodily fluid that naturally contains lots of potassium and creatinine. By estimating how much the blood had been diluted, the physicians calculated just how much urine had been introduced into each vial. The mother denied any wrongdoing when confronted by a psychiatrist, and child protective services intervened.
Other horror stories abound--patients who inject saliva, water, and even feces into their bloodstream, mothers (most people with Munchausen syndrome are females) who repeatedly suffocate their children. The diagnosis is extremely difficult to make, because the patient is deftly and secretly conspiring against the doctor.
The physicians in the case I described put it well: "It seems that in the case of Munchausen-by-proxy syndrome, the perpetrator may be more creative than physicians can imagine."
Some of the most befuddling and tragic "con men" a doctor will see are those with Munchausen syndrome, who intentionally exaggerate, induce, or simulate illness or injury, in order "to assume the sick role." Munchausen syndrome by proxy occurs when someone intentionally induces or simulates injury in another (typically their child).
Diagnosing a patient can sometimes be like answering a trick question: the ordinary rules don't always apply. A case report in the NEJM reads like a detective story. A healthy-seeming toddler presented to a clinic because of a "reported febrile convulsion." Blood samples were taken on several occasions and given to the patient's mother, who dropped them off at the laboratory for processing. Each one showed potassium and creatinine levels so high as to be "incompatible with life." This apparently piqued the interest of the physicians, who recognized that the readings were factitious (not reflective of reality).
The doctors readminstered the blood test and gave the mother two blood samples with her daughter's name on it--except that one secretly contained a different patient's blood whose lab values were known. Sure enough, both blood samples came back with impossibly high potassium and creatinine levels.
The physicians knew of another bodily fluid that naturally contains lots of potassium and creatinine. By estimating how much the blood had been diluted, the physicians calculated just how much urine had been introduced into each vial. The mother denied any wrongdoing when confronted by a psychiatrist, and child protective services intervened.
Other horror stories abound--patients who inject saliva, water, and even feces into their bloodstream, mothers (most people with Munchausen syndrome are females) who repeatedly suffocate their children. The diagnosis is extremely difficult to make, because the patient is deftly and secretly conspiring against the doctor.
The physicians in the case I described put it well: "It seems that in the case of Munchausen-by-proxy syndrome, the perpetrator may be more creative than physicians can imagine."
18 September 2011
They know their customers
I recently noticed that our school's vending machines stock "Red Bull" and "Rockstar" energy drinks. They seem to sell out right around exam time.
What's next, caffeine tablets?
What's next, caffeine tablets?
11 September 2011
Redundancy
I just got back from watching "Contagion", Stephen Sondheim's hyper-realistic and emotionless portrayal of a fictional pandemic. I wasn't wild enough about the film to recommend it, but it brings up many points that merit further discussion. One of these is the film's portrayal of badly-overcrowded hospitals.
A pandemic's overwhelming demand on the medical system is a very real concern. Doctors are rather busy people even during periods of ordinary demand on the medical system. Medical residents work close to 80 hours a week, and hospitals try to keep their patient load as close to full-capacity as possible (they aren't so different from businesses, after all). Pandemics can quickly use up medical supplies, sparking shortages of body bags, ventilators, and antivirals. They tax medical systems designed to be running as close to capacity as possible.
Worse still, front-line medical workers are some of the likeliest to catch pandemic disease, because of their exposure to ill patients. Some medical workers will not want to come into work, for fear of catching the disease or spreading it to their families.
How to respond to these sudden demands? During the 1918 influenza pandemic, student nurses, medical students, retired medical personnel, and the barely-trained or untrained endeavored to fill the gaps in the medical system. We potentially could expand the scope of care to allow podiatrists, veterinarians, and nurses to treat patients without supervision during crises.
A more systemic fix is to incorporate more redundancy into the medical system and expand its capacity. Residents would work fewer hours, hospitals would have extra beds and operating rooms, equipment would be stockpiled. Although this would require extra cost, the trade-off is that it might pay off tremendously when we need it most.
A pandemic's overwhelming demand on the medical system is a very real concern. Doctors are rather busy people even during periods of ordinary demand on the medical system. Medical residents work close to 80 hours a week, and hospitals try to keep their patient load as close to full-capacity as possible (they aren't so different from businesses, after all). Pandemics can quickly use up medical supplies, sparking shortages of body bags, ventilators, and antivirals. They tax medical systems designed to be running as close to capacity as possible.
Worse still, front-line medical workers are some of the likeliest to catch pandemic disease, because of their exposure to ill patients. Some medical workers will not want to come into work, for fear of catching the disease or spreading it to their families.
How to respond to these sudden demands? During the 1918 influenza pandemic, student nurses, medical students, retired medical personnel, and the barely-trained or untrained endeavored to fill the gaps in the medical system. We potentially could expand the scope of care to allow podiatrists, veterinarians, and nurses to treat patients without supervision during crises.
A more systemic fix is to incorporate more redundancy into the medical system and expand its capacity. Residents would work fewer hours, hospitals would have extra beds and operating rooms, equipment would be stockpiled. Although this would require extra cost, the trade-off is that it might pay off tremendously when we need it most.
07 September 2011
Who needs sleep?
In a piece for the New York Times online, a nurse explores why hospitals are not set up to let patients sleep. It's an interesting read.
One thing the author doesn't mention are private rooms, which really help patients get a good night's sleep. My impression is that these are becoming increasingly common in hospitals.
One thing the author doesn't mention are private rooms, which really help patients get a good night's sleep. My impression is that these are becoming increasingly common in hospitals.
05 September 2011
Disaster averted
I've been transfixed by the National Hurricane Center's ongoing updates and forecasts of tropical cyclones.
Unlike most natural disasters, our government gives cities several days' warning before they are struck by a hurricane. Patients in some New York City hospitals were evacuated well before Hurricane Irene arrived, avoiding the harrowing scene grippingly recounted by ER physician Kevin Kitka, who was working in a Joplin, Mo. hospital when a large tornado hit.
Unlike most natural disasters, our government gives cities several days' warning before they are struck by a hurricane. Patients in some New York City hospitals were evacuated well before Hurricane Irene arrived, avoiding the harrowing scene grippingly recounted by ER physician Kevin Kitka, who was working in a Joplin, Mo. hospital when a large tornado hit.
04 September 2011
Clinical notes
The patient was 44 years old and had an uncontrollable, Parkinson-like tremor in both hands that had been worsening for months. His shaking hands were getting in the way of his manual-labor job and made everyday tasks such as clothing himself and brushing his teeth nearly impossible.
It's almost inexplicable for someone so young to develop Parkinson's. Something else had to be at play--the patient's longtime meth use, which he had unsuccessfully tried to break and which he hid from his family. Now the drug had caught up with him, causing what was likely permanent damage to his brain. The news that the meth was jeopardizing his ability to support his family came as a sobering shock. When the physician informed him that he must never take another dose of meth, ever, the patient teared up, gravely agreed, and vowed to change.
Everyone in the exam room was touched by this patient, who was quite likeable and was trapped and diminished by addiction. He had persevered in the face of past obstacles, and had tried to do good for himself and his family. Now, his own worst enemy was himself, and only through sheer willpower could he stop his demon from claiming more of his body.
It's almost inexplicable for someone so young to develop Parkinson's. Something else had to be at play--the patient's longtime meth use, which he had unsuccessfully tried to break and which he hid from his family. Now the drug had caught up with him, causing what was likely permanent damage to his brain. The news that the meth was jeopardizing his ability to support his family came as a sobering shock. When the physician informed him that he must never take another dose of meth, ever, the patient teared up, gravely agreed, and vowed to change.
Everyone in the exam room was touched by this patient, who was quite likeable and was trapped and diminished by addiction. He had persevered in the face of past obstacles, and had tried to do good for himself and his family. Now, his own worst enemy was himself, and only through sheer willpower could he stop his demon from claiming more of his body.
03 September 2011
A crime
James Verone of Gastonia, N.C. was 59 years old when he noticed a lump growing out of his chest. He had been laid off from his job of 17 years working as a delivery truck driver and hadn't managed to find steady work since. He lacked health insurance. Recognizing that he needed care, he decided to rob a bank for $1, just so that he would be sent to prison and receive treatment.
“I'm sort of a logical person and that was my logic. [This is] what I came up with,” Verone told a North Carolina news station. He had no past criminal record.
It's hard to argue with Verone's thinking (what would you do in his shoes?). It's a truly sorry state of affairs. And since the government is paying for Verone's health care anyway, it is a costly folly that he will be incarcerated as well when he could have been a productive member of society.
Most of the Affordable Care Act's improvements to the insurance system are slated to take effect in 2015. Yet many obstacles remain. Recent federal court decisions, pressure from governors, and a threat of repeal from Republican Congressmen threaten to undo several key provisions. I'm still hoping that universal health care will triumph.
“I'm sort of a logical person and that was my logic. [This is] what I came up with,” Verone told a North Carolina news station. He had no past criminal record.
It's hard to argue with Verone's thinking (what would you do in his shoes?). It's a truly sorry state of affairs. And since the government is paying for Verone's health care anyway, it is a costly folly that he will be incarcerated as well when he could have been a productive member of society.
Most of the Affordable Care Act's improvements to the insurance system are slated to take effect in 2015. Yet many obstacles remain. Recent federal court decisions, pressure from governors, and a threat of repeal from Republican Congressmen threaten to undo several key provisions. I'm still hoping that universal health care will triumph.
01 September 2011
How bad is it out there?
What is life like in a place without many fruits and vegetables available? The Internets Celebrities are hard to classify--they are three guys from the Bronx who make funny documentaries about serious stuff. Some years ago, they chronicled their neighborhood bodega:
Is obesity really such a problem in America today? Emphatically, yes.
I encourage you to play the CDC's slideshow on obesity by state over the past 25 years. Although Colorado currently has the lowest obesity rate in the country, its current obesity rate would have made it the fattest state in the country in 1996.
The CDC's county-by-county statistics are sobering. Some counties in Alabama and Mississippi have upwards of 40% obesity among adults. And the costs, from higher fuel costs for fatter passengers to exploding health expenditures, are accruing quickly.
But I don't feel like I see many obese people when I go around town. My time in hospital and clinic is teaching me that many are tucked out of sight, at home, in hospitals, and in nursing facilities. Obesity makes walking around more difficult (or impossible), and the social stigma against obesity makes some people reluctant to leave the house. But they are there, their ranks are growing, and the medical profession has few tools to treat (let alone cure) obesity. There is an urgent need to act.
Is obesity really such a problem in America today? Emphatically, yes.
I encourage you to play the CDC's slideshow on obesity by state over the past 25 years. Although Colorado currently has the lowest obesity rate in the country, its current obesity rate would have made it the fattest state in the country in 1996.
The CDC's county-by-county statistics are sobering. Some counties in Alabama and Mississippi have upwards of 40% obesity among adults. And the costs, from higher fuel costs for fatter passengers to exploding health expenditures, are accruing quickly.
But I don't feel like I see many obese people when I go around town. My time in hospital and clinic is teaching me that many are tucked out of sight, at home, in hospitals, and in nursing facilities. Obesity makes walking around more difficult (or impossible), and the social stigma against obesity makes some people reluctant to leave the house. But they are there, their ranks are growing, and the medical profession has few tools to treat (let alone cure) obesity. There is an urgent need to act.
31 August 2011
The trouble with obesity
What difference does it make if one person is obese instead of thin? More than you might suppose.
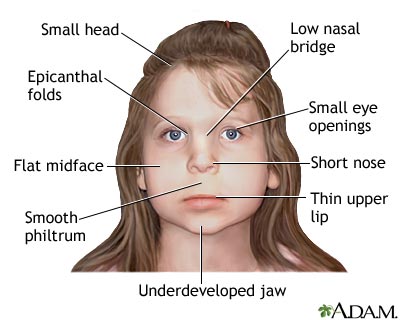 Our prenatal environment (the environment of the womb) has an outsized effect on our development. For example, drinking even modest amounts of alcohol during pregnancy can cause fetal alcohol syndrome, which includes mental retardation, stunted growth, and disfigurement of facial features (see diagram at right).
Our prenatal environment (the environment of the womb) has an outsized effect on our development. For example, drinking even modest amounts of alcohol during pregnancy can cause fetal alcohol syndrome, which includes mental retardation, stunted growth, and disfigurement of facial features (see diagram at right).
The environment of an obese woman's womb (especially one with diabetes) tends to be injurious to a fetus's metabolism. For example, a fetus will react to high placental blood sugar levels by stimulating insulin production in the pancreas or by becoming resistant to insulin. These steps apparently predispose the baby to become diabetic later in life. Among other things, being born to a obese mother makes a baby more likely to get diabetes, to have asthma, and to become obese later in life. It's not just children, either, who are affected. A convincing study in the New England Journal of Medicine suggests that when someone becomes obese during a certain interval, it makes their friends significantly more likely to become obese as well.
Preventing a patient's obesity can mean preventing their children's, grandchildren's, and friends' obesity as well. All the more incentive to act now to reverse the worldwide obesity epidemic.
[Image is in the public domain, via the NIH's A.D.A.M. medical encyclopedia]
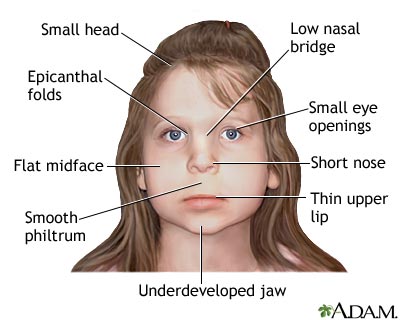 Our prenatal environment (the environment of the womb) has an outsized effect on our development. For example, drinking even modest amounts of alcohol during pregnancy can cause fetal alcohol syndrome, which includes mental retardation, stunted growth, and disfigurement of facial features (see diagram at right).
Our prenatal environment (the environment of the womb) has an outsized effect on our development. For example, drinking even modest amounts of alcohol during pregnancy can cause fetal alcohol syndrome, which includes mental retardation, stunted growth, and disfigurement of facial features (see diagram at right).The environment of an obese woman's womb (especially one with diabetes) tends to be injurious to a fetus's metabolism. For example, a fetus will react to high placental blood sugar levels by stimulating insulin production in the pancreas or by becoming resistant to insulin. These steps apparently predispose the baby to become diabetic later in life. Among other things, being born to a obese mother makes a baby more likely to get diabetes, to have asthma, and to become obese later in life. It's not just children, either, who are affected. A convincing study in the New England Journal of Medicine suggests that when someone becomes obese during a certain interval, it makes their friends significantly more likely to become obese as well.
Preventing a patient's obesity can mean preventing their children's, grandchildren's, and friends' obesity as well. All the more incentive to act now to reverse the worldwide obesity epidemic.
[Image is in the public domain, via the NIH's A.D.A.M. medical encyclopedia]
30 August 2011
Non-judgmental regard
On July 24, 1998, a psychotic schizophrenic gunman entered a side entrance at the U.S. Capitol. As he approached Representative John DeLay's office, he exchanged fire with two Capitol Police officers who later died of their wounds. The gunman was badly wounded as well.
Senator Bill Frist, a cardiologist, was leaving the Capitol when Congressional aides informed him that some men needed urgent medical assistance.
A New York Times article tells more of the story:
The story encapsulates what I find to be the most extraordinary and difficult tenet of modern medical ethics: "non-judgmental regard." Physicians are supposed to take patients exactly as they are, without judging or discriminating. In principle, then, the armed robber and the man he injured, in neighboring beds in the ER, are provided the same degree of care. The morbidly obese smoker with a heart attack should be treated with the same earnestness as the thin one. Judgments of worth or character are independent of treatment.
Non-judgmental regard can show the best of humanity. The medical journal Lancet offered a first-hand account of the conditions in Libyan hospitals at the front lines of their civil war (PubMed citation here; institutional access needed). Although the doctor-journalist worked in a hospital run by rebels, many patients were pro-Gaddafi soldiers, who were provided the same level of comfort and care as every other patient.
Because I've decided to become a medical student, I have to make medicine's ethical precepts my own. But I have a difficult time with shedding judgment. I don't treat people equally in my own life. I have friends, acquaintances, and enemies, and I care about some of them more than others. In clinic, some patients' stories touch me more than others'. One patient had developed a crippling Parkinsonian tremor, probably secondary to his addiction to meth that he had tried and failed to kick. His circumstances were wrenching and I especially wanted to help this man. My next patient, a woman with conjunctivitis who lambasted me for fumbling at first with the blood pressure cuff, was less inspiring. Some patients are especially kind to me in a way that I particularly want to reciprocate.
Don't all doctors necessarily judge patients differently? How would one diagnose Munchausen's if one unquestioningly believed the patient's narrative? For that matter, doesn't specializing mean deciding that a certain class of ailments matter more to you than another?
I'm not sure that "non-judgmental regard" is utopian or a necessary precept of medical practice. In a world where no one was judged, there would be no such thing as justice, morals, ethics, or a need for self-improvement. Humanity is rich and varied--why not treat it as such?
There are two worthy attitudes here: respecting each person equally and accepting them as they are; and being sympathetic and rewarding kindness with kindness. Are they mutually exclusive, or can they dovetail?
Senator Bill Frist, a cardiologist, was leaving the Capitol when Congressional aides informed him that some men needed urgent medical assistance.
A New York Times article tells more of the story:
[Frist] took off his coat and ran past the police barricade. ''I'm Senator Frist,'' he told an officer, flashing his ID. ''I'm a doctor.''
The police, still fearing there was more than one shooter, ushered him down a long marble corridor that smelled of gunpowder. He knelt by the first victim, checking his wounds and inserting a breathing tube. He lifted him on a stretcher and assisted paramedics as they wheeled him into an ambulance. But before they could close the door, the patient went into cardiac arrest. Although Frist helped to shock back his heartbeat, he was certain the man would die from his injuries.
A medic yelled that there were more victims inside, and Frist rushed back into the building to treat another of the wounded, a slight man who was lying on the carpet and bleeding heavily. An artery in his chest was severed, and Frist concentrated on stemming the flow of blood. He then rode along with him in the ambulance, keeping him alive by forcing oxygen into his lungs. Only as they approached the hospital did he learn that the man he had rescued was the accused gunman, Russell Weston Jr. ''You're not a judge; you're not a jury,'' Frist later explained. ''You're a physician.''
Non-judgmental regard can show the best of humanity. The medical journal Lancet offered a first-hand account of the conditions in Libyan hospitals at the front lines of their civil war (PubMed citation here; institutional access needed). Although the doctor-journalist worked in a hospital run by rebels, many patients were pro-Gaddafi soldiers, who were provided the same level of comfort and care as every other patient.
Because I've decided to become a medical student, I have to make medicine's ethical precepts my own. But I have a difficult time with shedding judgment. I don't treat people equally in my own life. I have friends, acquaintances, and enemies, and I care about some of them more than others. In clinic, some patients' stories touch me more than others'. One patient had developed a crippling Parkinsonian tremor, probably secondary to his addiction to meth that he had tried and failed to kick. His circumstances were wrenching and I especially wanted to help this man. My next patient, a woman with conjunctivitis who lambasted me for fumbling at first with the blood pressure cuff, was less inspiring. Some patients are especially kind to me in a way that I particularly want to reciprocate.
Don't all doctors necessarily judge patients differently? How would one diagnose Munchausen's if one unquestioningly believed the patient's narrative? For that matter, doesn't specializing mean deciding that a certain class of ailments matter more to you than another?
I'm not sure that "non-judgmental regard" is utopian or a necessary precept of medical practice. In a world where no one was judged, there would be no such thing as justice, morals, ethics, or a need for self-improvement. Humanity is rich and varied--why not treat it as such?
There are two worthy attitudes here: respecting each person equally and accepting them as they are; and being sympathetic and rewarding kindness with kindness. Are they mutually exclusive, or can they dovetail?
29 August 2011
Beware of fair concessionaires' fare
TV crews reporting on the political candidates and Republican straw poll at Iowa's state fair introduced the country to the boldest frontier in fattening cuisine: deep-fried butter on a stick. In case you haven't been keeping on top of your deep-fried confections, Gawker has an enlightening video from an Iowan TV station.
It's also worth noting that the Center for Science in the Public Interest released its annual Xtreme eating awards. The awards are given to restaurants with the most insanely unhealthy menu items (this year's winners include a 2,010 calorie Cold Stone milkshake and an Applebee's pasta dish with 3,700 milligrams of sodium). I actually ate some of the Red Velvet Cake Cheescake from the Cheesecake Factory, and I can verify that the frosting really is pure cream cheese.
It's hard to stay motivated to read my textbooks on keeping people healthy when I can picture my nemeses, including KFC's culinary team, dreaming up the newest ways to jam salt and saturated fat onto their customers' trays. Is the war already lost?
It's also worth noting that the Center for Science in the Public Interest released its annual Xtreme eating awards. The awards are given to restaurants with the most insanely unhealthy menu items (this year's winners include a 2,010 calorie Cold Stone milkshake and an Applebee's pasta dish with 3,700 milligrams of sodium). I actually ate some of the Red Velvet Cake Cheescake from the Cheesecake Factory, and I can verify that the frosting really is pure cream cheese.
It's hard to stay motivated to read my textbooks on keeping people healthy when I can picture my nemeses, including KFC's culinary team, dreaming up the newest ways to jam salt and saturated fat onto their customers' trays. Is the war already lost?
27 August 2011
Issues with shoes
My patient, a homeless man in decent health, came to our volunteer clinic because he had "athlete's foot" and wanted an anti-fungal.
When I asked him to remove his shoes and socks so I could take a look, he refused. I pointed out that most doctors won't write a prescription for something unless they can examine it. He still refused and wouldn't say why. He cooperated with the other parts of the exam.
I brought in the attending physician, who asked to look at the foot. No dice. The physician and I conferred:
What's going on here? Maybe he doesn't have athlete's foot and he's getting it for a friend? Maybe it smells really bad and he's embarrassed?
We ultimately gave him a tube of prescription topical antifungal (we didn't have non-prescription). There isn't much you can do with antifungal cream (would it get you high if you snorted it?) and we didn't think there's much of a black market for Lamisil. We probably helped someone's athlete's foot, although who knows if it was the patient's.
I don't know which is more incredible: that the patient thought he could get anti-fungals without showing us his foot, or that he got just that.
When I asked him to remove his shoes and socks so I could take a look, he refused. I pointed out that most doctors won't write a prescription for something unless they can examine it. He still refused and wouldn't say why. He cooperated with the other parts of the exam.
I brought in the attending physician, who asked to look at the foot. No dice. The physician and I conferred:
What's going on here? Maybe he doesn't have athlete's foot and he's getting it for a friend? Maybe it smells really bad and he's embarrassed?
We ultimately gave him a tube of prescription topical antifungal (we didn't have non-prescription). There isn't much you can do with antifungal cream (would it get you high if you snorted it?) and we didn't think there's much of a black market for Lamisil. We probably helped someone's athlete's foot, although who knows if it was the patient's.
I don't know which is more incredible: that the patient thought he could get anti-fungals without showing us his foot, or that he got just that.
21 August 2011
A morning on the wards
An internal medicine hospitalist (a physician who cares solely for hospitalized adult patients who are not in the ICU) kindly took me along as he rounded on his patients. Together we went over his patients' lab results, imaging studies, and medical histories and then traversed the wards to check on them.
I knew that hospitalized patients ("inpatients") would be sicker than the patients I saw in outpatient clinic. But it was more sobering than I expected interacting with them and learning the extent of their illnesses. Examples of frequent medical issues during the three hours I was on the wards:
-incurable metastatic cancer
-severe and irreversible breathing problems, brought on by smoking tobacco, smoking cocaine, morbid obesity, exposure to Agent Orange, and venous blood clots that had migrated to the lungs ("pulmonary embolism")
-dementia and delirium; whether because of denial or cognitive impairments, many patients were largely unaware of their diagnoses and their treatment plans.
-urinary incontinence and constipation (a side-effect of the high doses of painkillers the patients required).
-a lack of a support network; one patient can't be discharged until the hospital can find a skilled nursing facility to house him, with no resolution in sight.
Most patients were either getting worse or staying the same. The physician had to inform several patients that the end was drawing near. One patient, who understood he was seriously ill but had a decent chance of recovery, asked hoarsely if we could "do a Kevorkian" on him. The hospitalist's response was perfect: "Not going to happen. Kevorkian was a Michigan guy, and I root for Ohio State because my kids go there for school." Instead, the hospitalist suggested that the patient change his "code status," so that medical staff would not perform CPR or place him on a ventilator should he stop breathing on his own. The patient's mood lightened, and the hospitalist secured his OK on continuing for now with aggressive treatment. Still, the patients were a depressed lot (and justifiably so, accompanied as they are by pain and the specter of death). It seemed that having family, friends, or some avenue of self-expression would have helped many of them considerably, but instead the TV was their sole means of escaping the monotony of the hospital room. If I wasn't scrambling to pay for med school, I'd be tempted to buy Etch-a-Sketches for the patients in the wards, just so they could do something creative.
I didn't shadow physicians before starting medical school (while nearly all successful med school applicants shadow as undergrads, I remain happy with my decision). I found it useful today as a medical student for several reasons:
1. It familiarizes me with the hospital and the medical records systems.
2. It gives me an understanding of what certain specialists' day-to-day routine looks like.
3. It introduces me to new medical knowledge and examination methods, and reinforces and ties together those that I already know.
4. It reminds me why this whole med school enterprise is worth it.
5. It exposes me to how a skilled clinician interacts with his patients. My hospitalist had to perform a delicate dance, of examining his patients, asking them good questions, listening to them, providing appropriate treatment (such as appropriate doses of pain meds) comforting them, and being mindful of the time constraints his schedule placed on him. He seemed to succeed, given how many patients confessed their past drug use, unprompted.
I was glad to see how grateful the patients were to my doctor. Many told him that they trust him, that he's a "good doc", or that he cares about him. Unfortunately, many of these remarks were followed by something along the lines of, "yeah, and all of those other doctors are really cold." A partial victory for the profession, but I'll take it.
One consistent theme, and a topic of a future post, is that most of the patients' diseases either were preventable (obesity, complications from smoking, blood clots due to lack of exercise) or could have been successfully treated had they been caught earlier (disseminated cancer, sleep apnea requiring tracheostomy). Better prevention, better public health measures, a more robust primary-care system, and a better support system (such as family members) would have made a world of difference to these patients, and perhaps could have avoided these unfortunate and unnecessary brushes with death. When I brought this up to the hospitalist, he said while he was painfully aware of this reality, he couldn't let it get to him. His relationship with the patient starts when they're admitted to the hospital. What he does is comfort and heal his hospitalized patients, regardless of why they're there, and then try to ensure that his patients will receive appropriate care once they've been discharged. Seems reasonable enough.
I knew that hospitalized patients ("inpatients") would be sicker than the patients I saw in outpatient clinic. But it was more sobering than I expected interacting with them and learning the extent of their illnesses. Examples of frequent medical issues during the three hours I was on the wards:
-incurable metastatic cancer
-severe and irreversible breathing problems, brought on by smoking tobacco, smoking cocaine, morbid obesity, exposure to Agent Orange, and venous blood clots that had migrated to the lungs ("pulmonary embolism")
-dementia and delirium; whether because of denial or cognitive impairments, many patients were largely unaware of their diagnoses and their treatment plans.
-urinary incontinence and constipation (a side-effect of the high doses of painkillers the patients required).
-a lack of a support network; one patient can't be discharged until the hospital can find a skilled nursing facility to house him, with no resolution in sight.
Most patients were either getting worse or staying the same. The physician had to inform several patients that the end was drawing near. One patient, who understood he was seriously ill but had a decent chance of recovery, asked hoarsely if we could "do a Kevorkian" on him. The hospitalist's response was perfect: "Not going to happen. Kevorkian was a Michigan guy, and I root for Ohio State because my kids go there for school." Instead, the hospitalist suggested that the patient change his "code status," so that medical staff would not perform CPR or place him on a ventilator should he stop breathing on his own. The patient's mood lightened, and the hospitalist secured his OK on continuing for now with aggressive treatment. Still, the patients were a depressed lot (and justifiably so, accompanied as they are by pain and the specter of death). It seemed that having family, friends, or some avenue of self-expression would have helped many of them considerably, but instead the TV was their sole means of escaping the monotony of the hospital room. If I wasn't scrambling to pay for med school, I'd be tempted to buy Etch-a-Sketches for the patients in the wards, just so they could do something creative.
I didn't shadow physicians before starting medical school (while nearly all successful med school applicants shadow as undergrads, I remain happy with my decision). I found it useful today as a medical student for several reasons:
1. It familiarizes me with the hospital and the medical records systems.
2. It gives me an understanding of what certain specialists' day-to-day routine looks like.
3. It introduces me to new medical knowledge and examination methods, and reinforces and ties together those that I already know.
4. It reminds me why this whole med school enterprise is worth it.
5. It exposes me to how a skilled clinician interacts with his patients. My hospitalist had to perform a delicate dance, of examining his patients, asking them good questions, listening to them, providing appropriate treatment (such as appropriate doses of pain meds) comforting them, and being mindful of the time constraints his schedule placed on him. He seemed to succeed, given how many patients confessed their past drug use, unprompted.
I was glad to see how grateful the patients were to my doctor. Many told him that they trust him, that he's a "good doc", or that he cares about him. Unfortunately, many of these remarks were followed by something along the lines of, "yeah, and all of those other doctors are really cold." A partial victory for the profession, but I'll take it.
One consistent theme, and a topic of a future post, is that most of the patients' diseases either were preventable (obesity, complications from smoking, blood clots due to lack of exercise) or could have been successfully treated had they been caught earlier (disseminated cancer, sleep apnea requiring tracheostomy). Better prevention, better public health measures, a more robust primary-care system, and a better support system (such as family members) would have made a world of difference to these patients, and perhaps could have avoided these unfortunate and unnecessary brushes with death. When I brought this up to the hospitalist, he said while he was painfully aware of this reality, he couldn't let it get to him. His relationship with the patient starts when they're admitted to the hospital. What he does is comfort and heal his hospitalized patients, regardless of why they're there, and then try to ensure that his patients will receive appropriate care once they've been discharged. Seems reasonable enough.
20 August 2011
A knot-able occurence
I continue to be amazed by what random pieces of knowledge from my past are coming in handy these days. The other day, the taut-line hitch I learned in the Boy Scouts saved me from spending anatomy lab in my boxers.
 While putting on my scrubs for anatomy lab in the changing room, I found to my horror that one end of the drawstring had somehow gotten pulled into the bottoms. In a panic, I yanked on the other end of the drawstring, burying the lost end even further into the no-mans'-land of my waistband. The scrubs are several sizes too big, and awkwardly clutching my bottoms (like one of the "cool" kids in my middle school with baggy pants) for the 5 minute walk to anatomy lab was all I could manage to keep them from falling down. Class was starting and dissection is difficult with only one hand free. What to do?
While putting on my scrubs for anatomy lab in the changing room, I found to my horror that one end of the drawstring had somehow gotten pulled into the bottoms. In a panic, I yanked on the other end of the drawstring, burying the lost end even further into the no-mans'-land of my waistband. The scrubs are several sizes too big, and awkwardly clutching my bottoms (like one of the "cool" kids in my middle school with baggy pants) for the 5 minute walk to anatomy lab was all I could manage to keep them from falling down. Class was starting and dissection is difficult with only one hand free. What to do?
I wiped the "grime" off of some dissection forceps and tried vainly to grab hold of the string. Somehow this made the situation even worse and probably smeared the inside of my scrubs with formaldehyde.
My salvation came in the form of some string that the lab provides for bundling muscles and tying together skin flaps. To tie the string into a belt, I used the taut-line hitch, which is pretty much the only knot I remember from my Scout days. Heck, I still have troubles with my shoes, which become untied so often that I've pretty much given up on them. The beauty of the taut-line is that it makes a very strong loop, the length of which can be simply adjusted even after the knot's been tied. Upon fashioning a belt that loosened and tightened, I was so proud of it that I was sad to have to tuck it out of sight under my scrub tops.
That night, the taut-line came to the rescue again when I fixed, using dental floss, the poorly-designed IKEA hanging file rack that holds my lecture notes. Now my notes smell refreshingly minty.
It's nice how med school draws together together loose ends from our pasts. I just hope some of my Scout training remains purely theoretical--like the merit badge requirement that involved jumping into a lake fully-clothed, inflating one's jeans and long-sleeve shirt, and using them as flotation devices. At least when that day comes I'll be prepared.
[Images are shown with permission via Creative Commons license: scrubs attributable to wenzday01, taut-line schematic attributable to David J. Fred]
 While putting on my scrubs for anatomy lab in the changing room, I found to my horror that one end of the drawstring had somehow gotten pulled into the bottoms. In a panic, I yanked on the other end of the drawstring, burying the lost end even further into the no-mans'-land of my waistband. The scrubs are several sizes too big, and awkwardly clutching my bottoms (like one of the "cool" kids in my middle school with baggy pants) for the 5 minute walk to anatomy lab was all I could manage to keep them from falling down. Class was starting and dissection is difficult with only one hand free. What to do?
While putting on my scrubs for anatomy lab in the changing room, I found to my horror that one end of the drawstring had somehow gotten pulled into the bottoms. In a panic, I yanked on the other end of the drawstring, burying the lost end even further into the no-mans'-land of my waistband. The scrubs are several sizes too big, and awkwardly clutching my bottoms (like one of the "cool" kids in my middle school with baggy pants) for the 5 minute walk to anatomy lab was all I could manage to keep them from falling down. Class was starting and dissection is difficult with only one hand free. What to do?I wiped the "grime" off of some dissection forceps and tried vainly to grab hold of the string. Somehow this made the situation even worse and probably smeared the inside of my scrubs with formaldehyde.
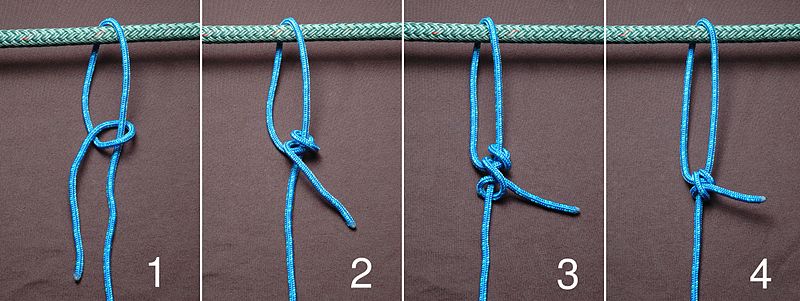 |
| The taut-line hitch |
That night, the taut-line came to the rescue again when I fixed, using dental floss, the poorly-designed IKEA hanging file rack that holds my lecture notes. Now my notes smell refreshingly minty.
It's nice how med school draws together together loose ends from our pasts. I just hope some of my Scout training remains purely theoretical--like the merit badge requirement that involved jumping into a lake fully-clothed, inflating one's jeans and long-sleeve shirt, and using them as flotation devices. At least when that day comes I'll be prepared.
[Images are shown with permission via Creative Commons license: scrubs attributable to wenzday01, taut-line schematic attributable to David J. Fred]
19 August 2011
Classes
The rumors were true: there is a lot of material to power through in medical school. One typical day consisted of five hour-long lectures:
-Signal transduction
-Disorders of hemoglobin
-Specialized epithelial glands
-Introduction to radiological techniques
-Interpreting radiological images of the spine
I'm impressed with both the depth and variety of topics discussed--we often have just a ten-minute break before we switch subjects entirely.
Following the lecture is usually a challenge--the material comes flying fast and some of us get lost partway through. Committing the information to memory is another trial. Whether or not I do a good job of assimilating the day's material (and I currently doubt that I am), the next day arrives and brings with it a whole new set of lectures.
The rigor exceeds that of my undergrad, which I felt was quite demanding. But it's awesome that med school offers an additional motivation to learn the material cold: the diseases our professors lecture us on may well present in a patient we see. Learning it properly may be the difference between bad care and good care, sickness and health.
-Signal transduction
-Disorders of hemoglobin
-Specialized epithelial glands
-Introduction to radiological techniques
-Interpreting radiological images of the spine
I'm impressed with both the depth and variety of topics discussed--we often have just a ten-minute break before we switch subjects entirely.
Following the lecture is usually a challenge--the material comes flying fast and some of us get lost partway through. Committing the information to memory is another trial. Whether or not I do a good job of assimilating the day's material (and I currently doubt that I am), the next day arrives and brings with it a whole new set of lectures.
The rigor exceeds that of my undergrad, which I felt was quite demanding. But it's awesome that med school offers an additional motivation to learn the material cold: the diseases our professors lecture us on may well present in a patient we see. Learning it properly may be the difference between bad care and good care, sickness and health.
18 August 2011
Hypertension, and my first patients
Though med school has barely begun, I've had the opportunity to don my white coat, stethoscope, and reflex hammer and examine a total of five patients in an outpatient setting. All five presented with high blood pressure, all five had previously been diagnosed with hypertension, and all five had stopped taking their hypertensive medications simply because they didn't feel like taking them anymore. It's a fitting condition for my first patients to have, in that hypertension exemplifies both the spirit and the limitations of medical practice.
My first patient was a friendly man with an all-too-common story--he was overweight, lacked health insurance, and had severe hypertension. Although he had been on drugs for hypertension in the distant past, he stopped taking his meds years ago because he felt better. He came to clinic because when he recently had his blood pressure checked, it was extremely high (the reading I obtained was a good 40 ticks higher than I had ever seen before). I sought out the supervising physician, who examined him, wrote some prescriptions, ordered some labs to see if his kidneys were damaged, and instructed him to return in a few weeks. I played pharmacist and gave him several weeks' supply of hypertensive drugs to get started.
Another patient had hypertension despite maintaining a good diet and healthy weight, as well as hypokalemia (too little potassium in the blood). The doctor suspected hyperaldosteronism (often, a tumor of the adrenal glands that overexpresses aldosterone, a hormone affecting blood pressure). Another was a fit teenage athlete with a clean bill of health, except for a menacingly high blood pressure of unknown etiology (unclear cause).
Technology gives us remarkable tools to combat hypertension. An easy-to-use, inexpensive, and reusable device (the sphygmomanometer, or blood pressure cuff) reliably diagnoses hypertension. You need not travel further than your local supermarket to check (within seconds! free!) whether the "silent killer" lurks in your arteries. But the most effective interventions are beyond medicine's grasp. Sure, we can prescribe diuretics and ACE inhibitors, but public health is best equipped to tackle the problems that usually cause or exacerbate hypertension--the shocking and indefensible amount of sodium in processed foods; and people eating poor diets, exercising too little, and weighing too much. Funding PE in schools or having the FDA follow through on its proposal to regulate salt in processed foods would far outstrip the concerted efforts of thousands of well-meaning doctors and medical students.
Telling the patient, "improve your diet" and "exercise more" doesn't help either. Two of my patients don't speak English--how are they going to figure out what foods have lower sodium when they go shopping? Another has no job--how will they pay for more expensive, but healthier foods? Another has a bad knee--how are they going to exercise?
So we prescribe them meds, and many patients take them for a few months and then stop. It's hard to blame them--while the drugs have side effects, hypertension feels fine. Like bad sunburns, the punishment for having high blood pressure is years or decades off. If a patient isn't motivated to make lifestyle changes to combat hypertension, how motivated will they be to stick with their meds?
The point is, science only gets the doctor so far. We understand the biochemical mechanism of hypertension, we understand how deadly it is, we can easily diagnose it, and we know how to cheaply and effectively treat and even prevent it. Yet hypertension still afflicts a third of adults in the U.S. and kills a substantial fraction of them. We can't escape the fact that patients are people, with people's foibles, strengths, and shortcomings. This makes treating chronic illness frustrating and sometimes ineffectual. But that I am dealing not just with kidneys and arteries and hearts, but with people, is what also makes clinical medicine intensely rewarding.
My first patient was a friendly man with an all-too-common story--he was overweight, lacked health insurance, and had severe hypertension. Although he had been on drugs for hypertension in the distant past, he stopped taking his meds years ago because he felt better. He came to clinic because when he recently had his blood pressure checked, it was extremely high (the reading I obtained was a good 40 ticks higher than I had ever seen before). I sought out the supervising physician, who examined him, wrote some prescriptions, ordered some labs to see if his kidneys were damaged, and instructed him to return in a few weeks. I played pharmacist and gave him several weeks' supply of hypertensive drugs to get started.
Another patient had hypertension despite maintaining a good diet and healthy weight, as well as hypokalemia (too little potassium in the blood). The doctor suspected hyperaldosteronism (often, a tumor of the adrenal glands that overexpresses aldosterone, a hormone affecting blood pressure). Another was a fit teenage athlete with a clean bill of health, except for a menacingly high blood pressure of unknown etiology (unclear cause).
Technology gives us remarkable tools to combat hypertension. An easy-to-use, inexpensive, and reusable device (the sphygmomanometer, or blood pressure cuff) reliably diagnoses hypertension. You need not travel further than your local supermarket to check (within seconds! free!) whether the "silent killer" lurks in your arteries. But the most effective interventions are beyond medicine's grasp. Sure, we can prescribe diuretics and ACE inhibitors, but public health is best equipped to tackle the problems that usually cause or exacerbate hypertension--the shocking and indefensible amount of sodium in processed foods; and people eating poor diets, exercising too little, and weighing too much. Funding PE in schools or having the FDA follow through on its proposal to regulate salt in processed foods would far outstrip the concerted efforts of thousands of well-meaning doctors and medical students.
Telling the patient, "improve your diet" and "exercise more" doesn't help either. Two of my patients don't speak English--how are they going to figure out what foods have lower sodium when they go shopping? Another has no job--how will they pay for more expensive, but healthier foods? Another has a bad knee--how are they going to exercise?
So we prescribe them meds, and many patients take them for a few months and then stop. It's hard to blame them--while the drugs have side effects, hypertension feels fine. Like bad sunburns, the punishment for having high blood pressure is years or decades off. If a patient isn't motivated to make lifestyle changes to combat hypertension, how motivated will they be to stick with their meds?
The point is, science only gets the doctor so far. We understand the biochemical mechanism of hypertension, we understand how deadly it is, we can easily diagnose it, and we know how to cheaply and effectively treat and even prevent it. Yet hypertension still afflicts a third of adults in the U.S. and kills a substantial fraction of them. We can't escape the fact that patients are people, with people's foibles, strengths, and shortcomings. This makes treating chronic illness frustrating and sometimes ineffectual. But that I am dealing not just with kidneys and arteries and hearts, but with people, is what also makes clinical medicine intensely rewarding.
Subscribe to:
Posts (Atom)