An internal medicine hospitalist (a physician who cares solely for hospitalized adult patients who are not in the ICU) kindly took me along as he rounded on his patients. Together we went over his patients' lab results, imaging studies, and medical histories and then traversed the wards to check on them.
I knew that hospitalized patients ("inpatients") would be sicker than the patients I saw in outpatient clinic. But it was more sobering than I expected interacting with them and learning the extent of their illnesses. Examples of frequent medical issues during the three hours I was on the wards:
-incurable metastatic cancer
-severe and irreversible breathing problems, brought on by smoking tobacco, smoking cocaine, morbid obesity, exposure to Agent Orange, and venous blood clots that had migrated to the lungs ("pulmonary embolism")
-dementia and delirium; whether because of denial or cognitive impairments, many patients were largely unaware of their diagnoses and their treatment plans.
-urinary incontinence and constipation (a side-effect of the high doses of painkillers the patients required).
-a lack of a support network; one patient can't be discharged until the hospital can find a skilled nursing facility to house him, with no resolution in sight.
Most patients were either getting worse or staying the same. The physician had to inform several patients that the end was drawing near. One patient, who understood he was seriously ill but had a decent chance of recovery, asked hoarsely if we could "do a Kevorkian" on him. The hospitalist's response was perfect: "Not going to happen. Kevorkian was a Michigan guy, and I root for Ohio State because my kids go there for school." Instead, the hospitalist suggested that the patient change his "code status," so that medical staff would not perform CPR or place him on a ventilator should he stop breathing on his own. The patient's mood lightened, and the hospitalist secured his OK on continuing for now with aggressive treatment. Still, the patients were a depressed lot (and justifiably so, accompanied as they are by pain and the specter of death). It seemed that having family, friends, or some avenue of self-expression would have helped many of them considerably, but instead the TV was their sole means of escaping the monotony of the hospital room. If I wasn't scrambling to pay for med school, I'd be tempted to buy Etch-a-Sketches for the patients in the wards, just so they could do something creative.
I didn't shadow physicians before starting medical school (while nearly all successful med school applicants shadow as undergrads, I remain happy with my decision). I found it useful today as a medical student for several reasons:
1. It familiarizes me with the hospital and the medical records systems.
2. It gives me an understanding of what certain specialists' day-to-day routine looks like.
3. It introduces me to new medical knowledge and examination methods, and reinforces and ties together those that I already know.
4. It reminds me why this whole med school enterprise is worth it.
5. It exposes me to how a skilled clinician interacts with his patients. My hospitalist had to perform a delicate dance, of examining his patients, asking them good questions, listening to them, providing appropriate treatment (such as appropriate doses of pain meds) comforting them, and being mindful of the time constraints his schedule placed on him. He seemed to succeed, given how many patients confessed their past drug use, unprompted.
I was glad to see how grateful the patients were to my doctor. Many told him that they trust him, that he's a "good doc", or that he cares about him. Unfortunately, many of these remarks were followed by something along the lines of, "yeah, and all of those other doctors are really cold." A partial victory for the profession, but I'll take it.
One consistent theme, and a topic of a future post, is that most of the patients' diseases either were preventable (obesity, complications from smoking, blood clots due to lack of exercise) or could have been successfully treated had they been caught earlier (disseminated cancer, sleep apnea requiring tracheostomy). Better prevention, better public health measures, a more robust primary-care system, and a better support system (such as family members) would have made a world of difference to these patients, and perhaps could have avoided these unfortunate and unnecessary brushes with death. When I brought this up to the hospitalist, he said while he was painfully aware of this reality, he couldn't let it get to him. His relationship with the patient starts when they're admitted to the hospital. What he does is comfort and heal his hospitalized patients, regardless of why they're there, and then try to ensure that his patients will receive appropriate care once they've been discharged. Seems reasonable enough.
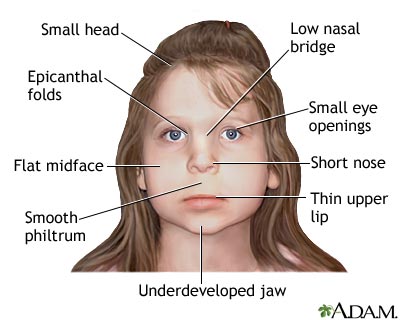 Our prenatal environment (the environment of the womb) has an outsized effect on our development. For example, drinking even modest amounts of alcohol during pregnancy can cause fetal alcohol syndrome, which includes mental retardation, stunted growth, and disfigurement of facial features (see diagram at right).
Our prenatal environment (the environment of the womb) has an outsized effect on our development. For example, drinking even modest amounts of alcohol during pregnancy can cause fetal alcohol syndrome, which includes mental retardation, stunted growth, and disfigurement of facial features (see diagram at right).