My heart sank and I swallowed nervously. I had just finished administering a vaccine for the second time ever, and the syringe's plunger felt strange as I finished pushing it in. It hit me. I had forgotten to check the vaccine for air bubbles, and I had injected a bit of air into my patient's left deltoid. I pictured him climbing into bed that night and dying of an air embolism, a cruel fate brought on by a vaccine that was supposed to protect from harm.
I tried to look calm and found an attending physician, who assured me that everything was fine. The amount of air in vaccines is miniscule, and in fact, having a bit of air in the syringe often helps an intramuscular injection. No harm done. But I was still shaken. Just like that, I had skipped a step that I had believed at the time to be critical.
The experience convinced me of just how easy it is to commit a medical error.
Even a simple procedure like administering a vaccine involves a number of important sequential steps. The sharps disposal container needs to be placed within arm's reach before the needle's cap is removed. The medical chart needs to be double-checked to ensure that the correct vaccination is being given. The injection site needs to be disinfected properly. Inevitably, even the best practitioners mess up a step. Medical errors are a tremendous problem, responsible for 48,000 to 98,000 deaths per year.
There is a growing movement to use checklists when carrying out medical procedures, just as pilots do when they fly. My favorite medical writer, Prof. Atul Gawande, wrote a fascinating article in the New Yorker on the subject, which I encourage you to read for free. Yes, individuals commit errors, yet the systems they work in can reduce the likelihood of those errors. For example, anesthesiology equipment wasn't standardized in the past, and turning a knob to the right would release more anesthetic on some machines and release less anesthetic on others. Now the equipment is consistent at every hospital in the country, avoiding needless deaths.
The fruits of prevention efforts are masked. When a hospital implements a labeling system to avoid wrong-side surgeries, patients who are saved won't know how narrowly they avoided catastrophe. It's not very obvious when the system succeeds, only when it fails. But even if prevention isn't sexy, we need to still try. Avoiding medical errors is inexpensive, it saves lives, and it is the right thing to do. For my part, I'm writing up a checklist for myself on how to administer vaccines properly.
Photo reproduced with permission via Creative Commons license. Author: @alviseni
27 September 2011
26 September 2011
An afternoon at elementary school
How familiar are inner-city kids with vegetables and healthy eating? I was pleasantly surprised to find out.
A classmate arranged for interested students to design and deliver an hour-long presentation about health at an inner-city elementary school. I signed up and received my assignment: first graders. How can anyone spend an hour discussing medicine with kids who can't tie their own shoes?
Lost, I turned to my brother for help. He challenged me to do something about obesity, sending along this must-see (but probably heavily-edited) video from Jamie Oliver's Food Revolution. The first-graders shown live in one of the most obese counties in the nation:
A challenge took shape: could my first-graders outdo their Huntington, West Virginia counterparts in identifying vegetables? With little more than a white coat, stethoscope, and zealous enthusiasm, could I inspire young children to improve their diets? My brother proposed a curriculum:
1. Explain how vegetables are a delicious and awesome part of a balanced diet.
2. Show various vegetables and see if students can identify them.
3. Have students draw a picture that has a vegetable in it.
4. Have students vote for their favorite vegetable.
5. Explain that anyone can be a doctor if they work hard in all subjects in school.
6. Feast on baby carrots.
I woke up early to snag exactly one of every vegetable from the local food co-op. My trip to the check-out portended badly for the vegetable quiz later that day, when the clerk and I disagreed over whether a root vegetable in my basket should be rung up as a leek or a garlic stalk.
A thoughtful classmate who is passionate about nutrition and excellent with kids thankfully offered to join me and split teaching duties. We drove to a rough part of town and found our school.
First graders say adorable things. Our presentation began something like this:
Med Student A: "We're medical students and we're here today to talk about vegetables! Vegetables are...yes, I see a hand."
Ashley: "One time, I got sick and I throwed up."
Med Student A: "Yes, that happens sometimes. Another question?"
Josiah: "My throat hurted...and...my dad made me eat ice."
Med Student B: "Yes! Ice can be good for you. So, about vegetables--"
Deidre: "I ate a banana yesterday for dinner."
Med Student B: "Awesome! I love bananas too! They're so delicious and good for you! So vegetables are..."
We eventually moved on to the quiz. Students successfully identified broccoli, carrots, cucumbers, and even eggplant. They displayed a surprisingly good grasp of what sorts of food were nutritious and which were not. They understood where vegetables grow, where they can be purchased, and even that you can grow your own vegetables in your garden and your yard. Our election crowned carrots as the crowd favorite, although ballot-stuffing plagued the polls. Unfortunately, "one man, one vote" is so foreign a concept that we tallied 50 votes among only 20 students. Fortunately, their math skills were so elementary (15 minus 11 was beyond their powers) that no one realized the election was a sham.
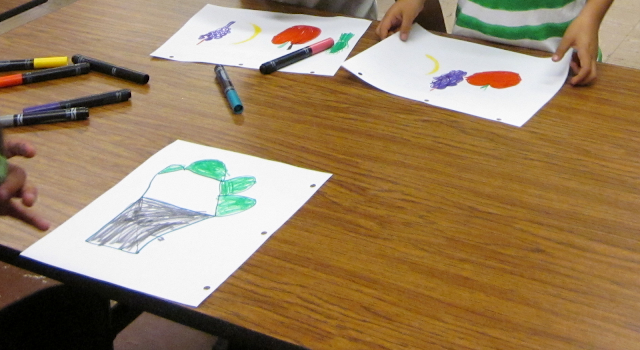
The students unleashed their creative juices and were keen to show us their handiwork. We saw plenty of fruits and vegetables as well as a few head-scratchers.
Annalise (holding up drawing): "What is this?"
Me: "That looks like a bunch of grapes!"
Annalise: "And this?"
Me: "That's a beautiful banana!"
Annalise: "What is this?"
Me: "Umm...I'm not really sure what that is. Is that an airplane?"
Annalise: "Aero-plane!"
It felt like I was doing improv acting again, where I had to heartily embrace all of my fellow actors' ideas (even when it meant portraying a crazed edentulous Gulf Coast fisherman) and encourage and support them. These young minds were delightfully bursting with creativity and non sequiturs.
At the end, it was time to feast on baby carrots. I have never seen kids so excited to eat carrots before. Even the kids on the playground, who we didn't teach at all, devoured our carrots after my fellow med student and I gushed over how delicious they are. Saturday morning cartoons are filled with advertisements successfully pushing sugary cereals and candy onto these malleable young minds. But this one wonderful afternoon, vegetables reigned king.
In the fight against obesity, there is hope after all.
A classmate arranged for interested students to design and deliver an hour-long presentation about health at an inner-city elementary school. I signed up and received my assignment: first graders. How can anyone spend an hour discussing medicine with kids who can't tie their own shoes?
Lost, I turned to my brother for help. He challenged me to do something about obesity, sending along this must-see (but probably heavily-edited) video from Jamie Oliver's Food Revolution. The first-graders shown live in one of the most obese counties in the nation:
A challenge took shape: could my first-graders outdo their Huntington, West Virginia counterparts in identifying vegetables? With little more than a white coat, stethoscope, and zealous enthusiasm, could I inspire young children to improve their diets? My brother proposed a curriculum:
1. Explain how vegetables are a delicious and awesome part of a balanced diet.
2. Show various vegetables and see if students can identify them.
3. Have students draw a picture that has a vegetable in it.
4. Have students vote for their favorite vegetable.
5. Explain that anyone can be a doctor if they work hard in all subjects in school.
6. Feast on baby carrots.
I woke up early to snag exactly one of every vegetable from the local food co-op. My trip to the check-out portended badly for the vegetable quiz later that day, when the clerk and I disagreed over whether a root vegetable in my basket should be rung up as a leek or a garlic stalk.
A thoughtful classmate who is passionate about nutrition and excellent with kids thankfully offered to join me and split teaching duties. We drove to a rough part of town and found our school.
First graders say adorable things. Our presentation began something like this:
Med Student A: "We're medical students and we're here today to talk about vegetables! Vegetables are...yes, I see a hand."
Ashley: "One time, I got sick and I throwed up."
Med Student A: "Yes, that happens sometimes. Another question?"
Josiah: "My throat hurted...and...my dad made me eat ice."
Med Student B: "Yes! Ice can be good for you. So, about vegetables--"
Deidre: "I ate a banana yesterday for dinner."
Med Student B: "Awesome! I love bananas too! They're so delicious and good for you! So vegetables are..."
We eventually moved on to the quiz. Students successfully identified broccoli, carrots, cucumbers, and even eggplant. They displayed a surprisingly good grasp of what sorts of food were nutritious and which were not. They understood where vegetables grow, where they can be purchased, and even that you can grow your own vegetables in your garden and your yard. Our election crowned carrots as the crowd favorite, although ballot-stuffing plagued the polls. Unfortunately, "one man, one vote" is so foreign a concept that we tallied 50 votes among only 20 students. Fortunately, their math skills were so elementary (15 minus 11 was beyond their powers) that no one realized the election was a sham.
 | |
| The election candidates |
The students unleashed their creative juices and were keen to show us their handiwork. We saw plenty of fruits and vegetables as well as a few head-scratchers.
Annalise (holding up drawing): "What is this?"
Me: "That looks like a bunch of grapes!"
Annalise: "And this?"
Me: "That's a beautiful banana!"
Annalise: "What is this?"
Me: "Umm...I'm not really sure what that is. Is that an airplane?"
Annalise: "Aero-plane!"
It felt like I was doing improv acting again, where I had to heartily embrace all of my fellow actors' ideas (even when it meant portraying a crazed edentulous Gulf Coast fisherman) and encourage and support them. These young minds were delightfully bursting with creativity and non sequiturs.
At the end, it was time to feast on baby carrots. I have never seen kids so excited to eat carrots before. Even the kids on the playground, who we didn't teach at all, devoured our carrots after my fellow med student and I gushed over how delicious they are. Saturday morning cartoons are filled with advertisements successfully pushing sugary cereals and candy onto these malleable young minds. But this one wonderful afternoon, vegetables reigned king.
In the fight against obesity, there is hope after all.
21 September 2011
The con man
Some of literature's most beloved characters thrive by cunningly misleading others (Odysseus, Don Juan, and Tom Sawyer come to mind). Yes, we scorn liars and con men, but we also celebrate those who have mastered the art of lies.
Some of the most befuddling and tragic "con men" a doctor will see are those with Munchausen syndrome, who intentionally exaggerate, induce, or simulate illness or injury, in order "to assume the sick role." Munchausen syndrome by proxy occurs when someone intentionally induces or simulates injury in another (typically their child).
Diagnosing a patient can sometimes be like answering a trick question: the ordinary rules don't always apply. A case report in the NEJM reads like a detective story. A healthy-seeming toddler presented to a clinic because of a "reported febrile convulsion." Blood samples were taken on several occasions and given to the patient's mother, who dropped them off at the laboratory for processing. Each one showed potassium and creatinine levels so high as to be "incompatible with life." This apparently piqued the interest of the physicians, who recognized that the readings were factitious (not reflective of reality).
The doctors readminstered the blood test and gave the mother two blood samples with her daughter's name on it--except that one secretly contained a different patient's blood whose lab values were known. Sure enough, both blood samples came back with impossibly high potassium and creatinine levels.
The physicians knew of another bodily fluid that naturally contains lots of potassium and creatinine. By estimating how much the blood had been diluted, the physicians calculated just how much urine had been introduced into each vial. The mother denied any wrongdoing when confronted by a psychiatrist, and child protective services intervened.
Other horror stories abound--patients who inject saliva, water, and even feces into their bloodstream, mothers (most people with Munchausen syndrome are females) who repeatedly suffocate their children. The diagnosis is extremely difficult to make, because the patient is deftly and secretly conspiring against the doctor.
The physicians in the case I described put it well: "It seems that in the case of Munchausen-by-proxy syndrome, the perpetrator may be more creative than physicians can imagine."
Some of the most befuddling and tragic "con men" a doctor will see are those with Munchausen syndrome, who intentionally exaggerate, induce, or simulate illness or injury, in order "to assume the sick role." Munchausen syndrome by proxy occurs when someone intentionally induces or simulates injury in another (typically their child).
Diagnosing a patient can sometimes be like answering a trick question: the ordinary rules don't always apply. A case report in the NEJM reads like a detective story. A healthy-seeming toddler presented to a clinic because of a "reported febrile convulsion." Blood samples were taken on several occasions and given to the patient's mother, who dropped them off at the laboratory for processing. Each one showed potassium and creatinine levels so high as to be "incompatible with life." This apparently piqued the interest of the physicians, who recognized that the readings were factitious (not reflective of reality).
The doctors readminstered the blood test and gave the mother two blood samples with her daughter's name on it--except that one secretly contained a different patient's blood whose lab values were known. Sure enough, both blood samples came back with impossibly high potassium and creatinine levels.
The physicians knew of another bodily fluid that naturally contains lots of potassium and creatinine. By estimating how much the blood had been diluted, the physicians calculated just how much urine had been introduced into each vial. The mother denied any wrongdoing when confronted by a psychiatrist, and child protective services intervened.
Other horror stories abound--patients who inject saliva, water, and even feces into their bloodstream, mothers (most people with Munchausen syndrome are females) who repeatedly suffocate their children. The diagnosis is extremely difficult to make, because the patient is deftly and secretly conspiring against the doctor.
The physicians in the case I described put it well: "It seems that in the case of Munchausen-by-proxy syndrome, the perpetrator may be more creative than physicians can imagine."
18 September 2011
They know their customers
I recently noticed that our school's vending machines stock "Red Bull" and "Rockstar" energy drinks. They seem to sell out right around exam time.
What's next, caffeine tablets?
What's next, caffeine tablets?
11 September 2011
Redundancy
I just got back from watching "Contagion", Stephen Sondheim's hyper-realistic and emotionless portrayal of a fictional pandemic. I wasn't wild enough about the film to recommend it, but it brings up many points that merit further discussion. One of these is the film's portrayal of badly-overcrowded hospitals.
A pandemic's overwhelming demand on the medical system is a very real concern. Doctors are rather busy people even during periods of ordinary demand on the medical system. Medical residents work close to 80 hours a week, and hospitals try to keep their patient load as close to full-capacity as possible (they aren't so different from businesses, after all). Pandemics can quickly use up medical supplies, sparking shortages of body bags, ventilators, and antivirals. They tax medical systems designed to be running as close to capacity as possible.
Worse still, front-line medical workers are some of the likeliest to catch pandemic disease, because of their exposure to ill patients. Some medical workers will not want to come into work, for fear of catching the disease or spreading it to their families.
How to respond to these sudden demands? During the 1918 influenza pandemic, student nurses, medical students, retired medical personnel, and the barely-trained or untrained endeavored to fill the gaps in the medical system. We potentially could expand the scope of care to allow podiatrists, veterinarians, and nurses to treat patients without supervision during crises.
A more systemic fix is to incorporate more redundancy into the medical system and expand its capacity. Residents would work fewer hours, hospitals would have extra beds and operating rooms, equipment would be stockpiled. Although this would require extra cost, the trade-off is that it might pay off tremendously when we need it most.
A pandemic's overwhelming demand on the medical system is a very real concern. Doctors are rather busy people even during periods of ordinary demand on the medical system. Medical residents work close to 80 hours a week, and hospitals try to keep their patient load as close to full-capacity as possible (they aren't so different from businesses, after all). Pandemics can quickly use up medical supplies, sparking shortages of body bags, ventilators, and antivirals. They tax medical systems designed to be running as close to capacity as possible.
Worse still, front-line medical workers are some of the likeliest to catch pandemic disease, because of their exposure to ill patients. Some medical workers will not want to come into work, for fear of catching the disease or spreading it to their families.
How to respond to these sudden demands? During the 1918 influenza pandemic, student nurses, medical students, retired medical personnel, and the barely-trained or untrained endeavored to fill the gaps in the medical system. We potentially could expand the scope of care to allow podiatrists, veterinarians, and nurses to treat patients without supervision during crises.
A more systemic fix is to incorporate more redundancy into the medical system and expand its capacity. Residents would work fewer hours, hospitals would have extra beds and operating rooms, equipment would be stockpiled. Although this would require extra cost, the trade-off is that it might pay off tremendously when we need it most.
07 September 2011
Who needs sleep?
In a piece for the New York Times online, a nurse explores why hospitals are not set up to let patients sleep. It's an interesting read.
One thing the author doesn't mention are private rooms, which really help patients get a good night's sleep. My impression is that these are becoming increasingly common in hospitals.
One thing the author doesn't mention are private rooms, which really help patients get a good night's sleep. My impression is that these are becoming increasingly common in hospitals.
05 September 2011
Disaster averted
I've been transfixed by the National Hurricane Center's ongoing updates and forecasts of tropical cyclones.
Unlike most natural disasters, our government gives cities several days' warning before they are struck by a hurricane. Patients in some New York City hospitals were evacuated well before Hurricane Irene arrived, avoiding the harrowing scene grippingly recounted by ER physician Kevin Kitka, who was working in a Joplin, Mo. hospital when a large tornado hit.
Unlike most natural disasters, our government gives cities several days' warning before they are struck by a hurricane. Patients in some New York City hospitals were evacuated well before Hurricane Irene arrived, avoiding the harrowing scene grippingly recounted by ER physician Kevin Kitka, who was working in a Joplin, Mo. hospital when a large tornado hit.
04 September 2011
Clinical notes
The patient was 44 years old and had an uncontrollable, Parkinson-like tremor in both hands that had been worsening for months. His shaking hands were getting in the way of his manual-labor job and made everyday tasks such as clothing himself and brushing his teeth nearly impossible.
It's almost inexplicable for someone so young to develop Parkinson's. Something else had to be at play--the patient's longtime meth use, which he had unsuccessfully tried to break and which he hid from his family. Now the drug had caught up with him, causing what was likely permanent damage to his brain. The news that the meth was jeopardizing his ability to support his family came as a sobering shock. When the physician informed him that he must never take another dose of meth, ever, the patient teared up, gravely agreed, and vowed to change.
Everyone in the exam room was touched by this patient, who was quite likeable and was trapped and diminished by addiction. He had persevered in the face of past obstacles, and had tried to do good for himself and his family. Now, his own worst enemy was himself, and only through sheer willpower could he stop his demon from claiming more of his body.
It's almost inexplicable for someone so young to develop Parkinson's. Something else had to be at play--the patient's longtime meth use, which he had unsuccessfully tried to break and which he hid from his family. Now the drug had caught up with him, causing what was likely permanent damage to his brain. The news that the meth was jeopardizing his ability to support his family came as a sobering shock. When the physician informed him that he must never take another dose of meth, ever, the patient teared up, gravely agreed, and vowed to change.
Everyone in the exam room was touched by this patient, who was quite likeable and was trapped and diminished by addiction. He had persevered in the face of past obstacles, and had tried to do good for himself and his family. Now, his own worst enemy was himself, and only through sheer willpower could he stop his demon from claiming more of his body.
03 September 2011
A crime
James Verone of Gastonia, N.C. was 59 years old when he noticed a lump growing out of his chest. He had been laid off from his job of 17 years working as a delivery truck driver and hadn't managed to find steady work since. He lacked health insurance. Recognizing that he needed care, he decided to rob a bank for $1, just so that he would be sent to prison and receive treatment.
“I'm sort of a logical person and that was my logic. [This is] what I came up with,” Verone told a North Carolina news station. He had no past criminal record.
It's hard to argue with Verone's thinking (what would you do in his shoes?). It's a truly sorry state of affairs. And since the government is paying for Verone's health care anyway, it is a costly folly that he will be incarcerated as well when he could have been a productive member of society.
Most of the Affordable Care Act's improvements to the insurance system are slated to take effect in 2015. Yet many obstacles remain. Recent federal court decisions, pressure from governors, and a threat of repeal from Republican Congressmen threaten to undo several key provisions. I'm still hoping that universal health care will triumph.
“I'm sort of a logical person and that was my logic. [This is] what I came up with,” Verone told a North Carolina news station. He had no past criminal record.
It's hard to argue with Verone's thinking (what would you do in his shoes?). It's a truly sorry state of affairs. And since the government is paying for Verone's health care anyway, it is a costly folly that he will be incarcerated as well when he could have been a productive member of society.
Most of the Affordable Care Act's improvements to the insurance system are slated to take effect in 2015. Yet many obstacles remain. Recent federal court decisions, pressure from governors, and a threat of repeal from Republican Congressmen threaten to undo several key provisions. I'm still hoping that universal health care will triumph.
01 September 2011
How bad is it out there?
What is life like in a place without many fruits and vegetables available? The Internets Celebrities are hard to classify--they are three guys from the Bronx who make funny documentaries about serious stuff. Some years ago, they chronicled their neighborhood bodega:
Is obesity really such a problem in America today? Emphatically, yes.
I encourage you to play the CDC's slideshow on obesity by state over the past 25 years. Although Colorado currently has the lowest obesity rate in the country, its current obesity rate would have made it the fattest state in the country in 1996.
The CDC's county-by-county statistics are sobering. Some counties in Alabama and Mississippi have upwards of 40% obesity among adults. And the costs, from higher fuel costs for fatter passengers to exploding health expenditures, are accruing quickly.
But I don't feel like I see many obese people when I go around town. My time in hospital and clinic is teaching me that many are tucked out of sight, at home, in hospitals, and in nursing facilities. Obesity makes walking around more difficult (or impossible), and the social stigma against obesity makes some people reluctant to leave the house. But they are there, their ranks are growing, and the medical profession has few tools to treat (let alone cure) obesity. There is an urgent need to act.
Is obesity really such a problem in America today? Emphatically, yes.
I encourage you to play the CDC's slideshow on obesity by state over the past 25 years. Although Colorado currently has the lowest obesity rate in the country, its current obesity rate would have made it the fattest state in the country in 1996.
The CDC's county-by-county statistics are sobering. Some counties in Alabama and Mississippi have upwards of 40% obesity among adults. And the costs, from higher fuel costs for fatter passengers to exploding health expenditures, are accruing quickly.
But I don't feel like I see many obese people when I go around town. My time in hospital and clinic is teaching me that many are tucked out of sight, at home, in hospitals, and in nursing facilities. Obesity makes walking around more difficult (or impossible), and the social stigma against obesity makes some people reluctant to leave the house. But they are there, their ranks are growing, and the medical profession has few tools to treat (let alone cure) obesity. There is an urgent need to act.
Subscribe to:
Comments (Atom)